Tech, Toys & Tools: A Brief Review of Health Tech's Most Popular

In today’s rapidly evolving health tech landscape, there is no shortage of innovative ideas, novel devices or digital health concepts. However, transforming a concept into a product that measurably improves health outcomes is a far more complex challenge. Numerous factors can delay or undermine even the most well intentioned efforts. Among these challenges for even the most promising product includes their reliance on perceived value and user adoption. Additional consideration of product market fit and regulatory hurdles only increase the competition in a market that often favors a small handful of dominant players. In the uniquely competitive world of health tech, clinical, behavioral and technological nuance often creates further challenge.
In this review, I examine some of the most widely adopted health tech products currently on the market, with a particular focus on their scientific credibility and real world efficacy. The goal is to assess not only what is popular, but what is proven through measurable impact on human health. Importantly, data driven feedback and baseline measurement technologies are only as valuable as the meaningful behavior change they inspire. Ultimately, it is this positive behavioral shift that provides the greatest benefit.

The Oura Ring, a clinically validated wearable, monitors key physiological metrics with a particular strength in sleep tracking. In my experience, and of my peers, it is most frequently utilized as a specialized sleep tool, even more so than for its other health features. This trend aligns with scientific findings as recent studies show strong agreement with Polysomnography (PSG), especially for total sleep time, REM sleep detection and the resulting readiness scores. Oura’s strength lies in transforming biometric data into personalized, actionable insights that encourage sustainable habit formation. Daily Readiness Scores incorporate key physiological markers to assess daily recovery and physical preparedness, further enabling users to make informed decisions. By providing consistent and personalized feedback, Oura empowers users to make data driven lifestyle decisions that promote long term health and well being.
Polysomnography (PSG) is the gold standard for detailed measurement of physiological activity during sleep. This comprehensive overnight study is primarily used to diagnose sleep disorders such as sleep apnea and narcolepsy. Often facilitated in a controlled sleep lab environment, PSG involves placing sensors on the various part of the body to monitor brain waves, eye movements, muscle activity, heart rate, breathing patterns, blood oxygen levels and body movements. While PSG provides unique insight into sleep stages, disruptions and overall physiological function, its complexity and dependance on specialized equipment make it impractical for routine or long term use outside clinical settings.
In contrast to the complexity of PSG, actigraphy is a validated, practical alternative for monitoring sleep and movement in real world environments over long periods of time. This approach uses non-invasive motion sensors to estimate sleep patterns based on activity levels, making it applicable in both clinical research and real world settings. The best example of this technology today is the increasingly popular Oura Ring, which enhances traditional actigraphy by integrating additional sensors that measure heart rate (HR), heart rate variability (HRV), body temperature and respiratory rate. By combining these multiple physiological signals, the Oura Ring provides a more comprehensive and nuanced assessment of sleep quality, recovery and overall health.
Notably, the Oura Ring also provides several lesser known physiological metrics that offer valuable insights often overlooked by users. The first is nighttime heart rate, which may be a more reliable indicator of sleep quality than commonly emphasized measures like deep sleep or REM duration. This is because heart rate reflects real time autonomic nervous system activity, while sleep stages are subject to broader interpretation. Ideally, the Oura Ring should display a downward trend in heart rate as the night progresses, reaching its lowest point during the early stages of deep sleep, followed by a gradual rise approaching wake time. Disruptions to this pattern, such as an elevated heart rate throughout the night, may signal poor recovery or suboptimal sleep. For example, exercise too close to bedtime can elevate heart rate and impair sleep quality. If this pattern is consistently observed, implementing routine changes or minimal effort sleep strategies can lead to meaningful improvements in sleep and overall health.

For individuals pursuing changes in body composition and weight loss, the Oura Ring’s body temperature metric can serve as a valuable physiological feedback tool, especially when combined with structured training, quality nutrition and adequate recovery. A consistently lower than baseline body temperature often reflects a sustained caloric deficit, whereas normal or elevated temperatures may indicate excess energy availability. While not a standalone diagnostic tool, this metric can function as a reliable data within a broader monitoring framework, informing modifications to physical activity or dietary intake. As highlighted in my previous article, If You (Don’t) Snooze, You Lose, body temperature also plays a critical role in sleep regulation, affecting one’s ability to initiate, maintain and cycle through sleep effectively. Importantly, sleep quality has been independently shown to influence body composition outcomes, both directly and indirectly.
The third and final metric is respiratory rate. Closely linked to autonomic nervous system activity, an elevated respiratory rate can reflect increased acute stress and heightened sympathetic nervous system dominance. For example, 16–18 breaths per minute may signal elevated sympathetic tone and is often associated with higher carbon dioxide (CO₂) levels, suggesting inefficient gas exchange or stress induced breathing patterns. In contrast, a lower respiratory rate typically reflects increased parasympathetic activation, a state supportive of rest and recovery. Fortunately, respiratory rate can be intentionally influenced. Through targeted breathing protocols, performance strategies or recovery interventions, one can shift autonomic tone toward their desired and optimal state. Consistently tracking respiratory rate offers a simple yet powerful insight into one's stress physiology and overall nervous system balance. For a deeper exploration of oxygen, CO₂ dynamics, and their significant impact on physical and cognitive performance, refer to my recent article, The Oxygen Advantage.

As health tools continue to gain traction, one product that has captured attention within the breathwork community (and in my own experience) is the Intake magnetic nasal band. Designed to enhance nasal airflow, these bands promote more efficient breathing by reducing resistance and encouraging consistent nasal inhalation. This supports the previously mentioned benefits associated with nasal breathing, including improved oxygen uptake, better autonomic regulation and enhanced respiratory efficiency. What makes these bands particularly appealing is their simplicity and the immediate, noticeable effects they offer, making them easy to integrate into daily routines. However, as with any health tool or practice, consistency remains the most important factor. The long term benefits of health tech tools are only realized through regular use and ongoing commitment. In my own routine, I've experienced significant benefits from using it during sleep, with improvements being validated through biometric feedback from my Oura Ring.
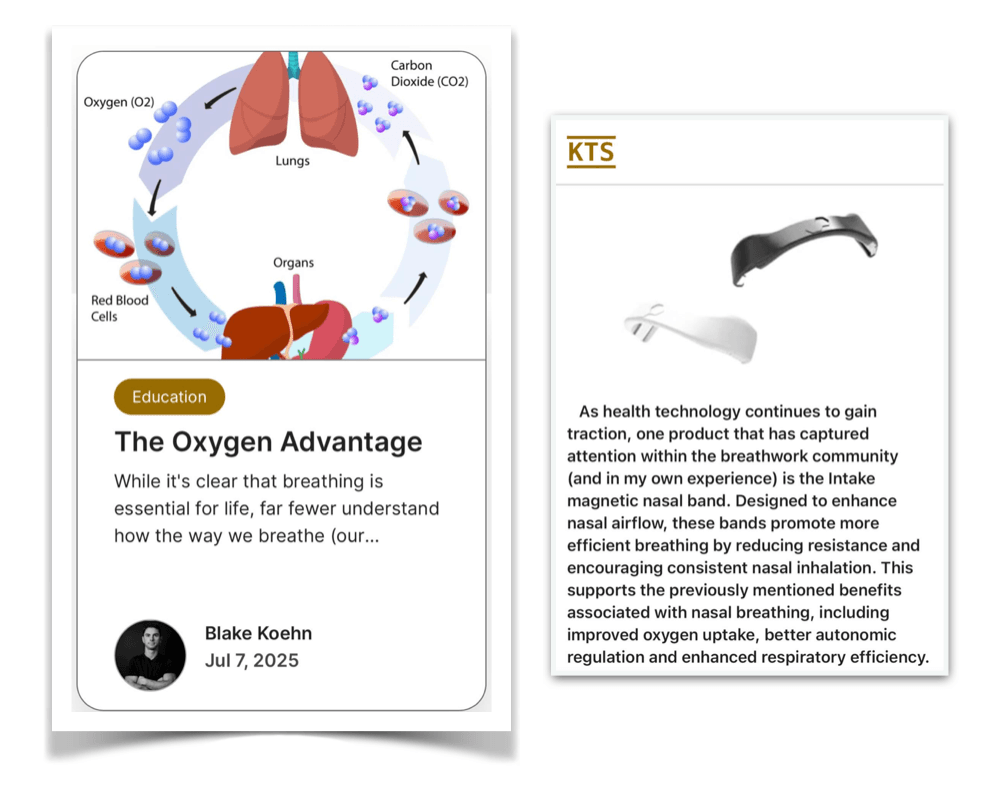
There is also a growing body of compelling evidence supporting the physiological advantages of nasal breathing over oral breathing. One study found that just five minutes of nasal breathing significantly lowered both mean and diastolic blood pressure compared to oral breathing, while systolic pressure and heart rate remained unchanged. Heart rate variability (HRV) analysis further revealed an increase in markers of enhanced parasympathetic nervous system activity and improved autonomic balance. Additionally, in a separate study involving 57 participants (including individuals with heart failure, chronic coronary syndrome and healthy controls across age groups), nasal breathing during submaximal exercise led to significantly greater ventilatory efficiency. This was reflected in a lower ventilation-to-carbon dioxide (V̇E/V̇CO₂) ratio, fewer breaths per minute, higher end-tidal CO₂ levels and increased tidal volumes, indicating deeper and more effective breathing. Collectively, these findings suggest that nasal breathing not only supports improved autonomic regulation at rest but also enhances respiratory mechanics and cardiovascular efficiency during physical exertion making it a powerful, accessible tool for sleep, health and performance.

The WHOOP band is an additional wearable designed to monitor key physiological metrics including HRV, resting HR, respiratory rate, sleep quality and physical strain. Independent studies have demonstrated that WHOOP provides valid and reliable HR and HRV measurements in free living conditions, showing strong agreement with electrocardiography (ECG) and PPG. Interestingly, WHOOP estimates HRV using the time-domain root mean square of successive differences (RMSSD) derived from photoplethysmography (PPG) signals collected during the final stages of sleep, an approach validated for its consistency under resting conditions. Its proprietary strain algorithm integrates cardiovascular load, duration and intensity to quantify the cumulative impact of physical and mental exertion on the body.
Heart rate variability (HRV) refers to the variation in time between successive heartbeats (the R-R intervals) and is a key marker of how well the autonomic nervous system is functioning. A higher HRV typically reflects a healthy balance between the sympathetic and parasympathetic nervous system, indicative of a well regulated stress response. WHOOP specifically collects HRV during periods of minimal movement (during slow wave sleep), when PPG signal noise is lowest. This strategic timing, along with advanced signal filtering and artifact rejection algorithms, improves the reliability of its HRV estimates. Because HRV is highly individual, tracking personal trends over time is more meaningful than comparing to others. Importantly, HRV is influenced by a range of factors, including age, fitness level, sleep quality, stress, hydration and overall health. Regular exercise, restorative sleep and low stress typically increase HRV, while illness, alcohol consumption, overtraining and emotional strain can lower it. HRV also naturally declines with age, emphasizing the importance of maintaining a consistently flat or stable HRV over time to retain cardiovascular fitness. Therefore, HRV measurements, whether in controlled lab settings or real world conditions, offer reliable, actionable feedback for improving physical performance, mental well being and overall health.
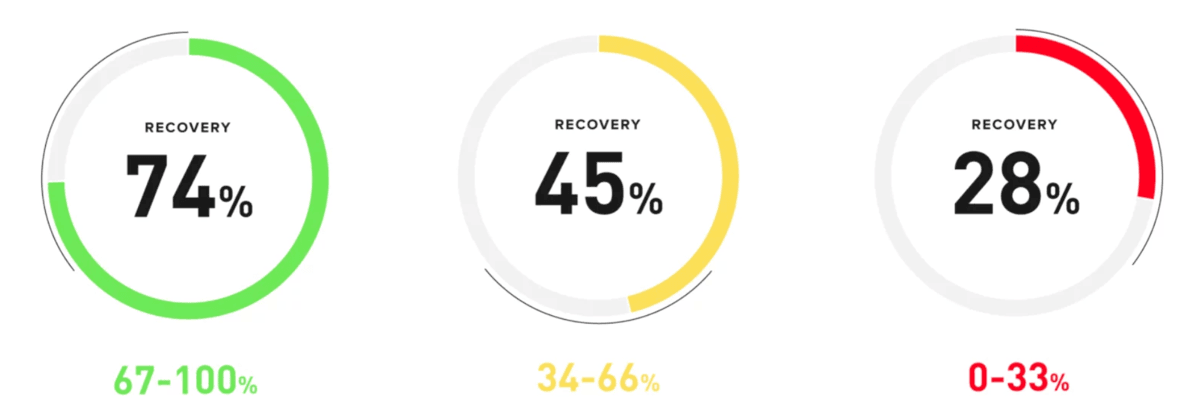
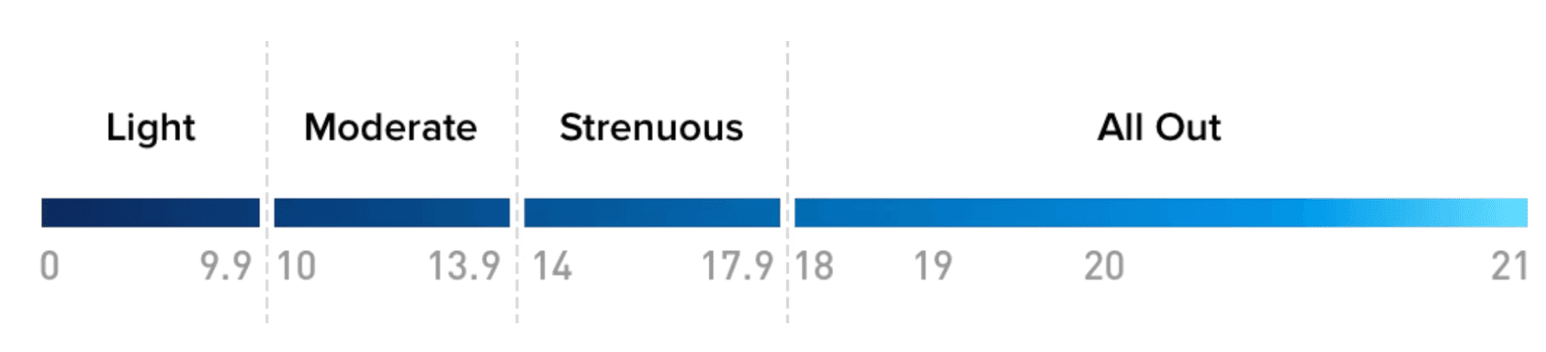
WHOOP calculates its strain score by continuously measuring HR to assess the intensity and duration of cardiovascular effort throughout the day. It personalizes this score based on individual HR zones and fitness levels, producing a value from 0 (minimal strain) to 21 (maximum exertion). This score helps users understand their daily cardiovascular load and informs recovery and training decisions. Photoplethysmography (PPG) is a widely used optical method in wearable technology that detects blood volume changes beneath the skin by measuring light absorption or reflection, allowing for the inference of heartbeats. WHOOP, and other similar wearables, use PPG to monitor HR and HRV with multiple studies showing strong agreement between these measurements and ECG data, particularly during rest and sleep when movement is minimal. Although motion artifacts and skin tone can affect accuracy during physical activity, PPG remains a scientifically validated, noninvasive and efficient method for continuous HR monitoring, making it the preferred standard in consumer health wearables.
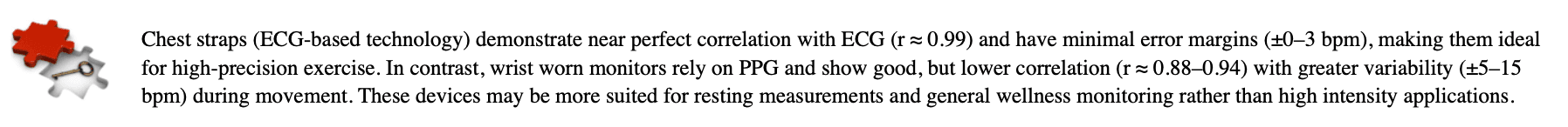
While the standard WHOOP model relies solely on PPG sensors for continuous tracking of HR, HRV, sleep and strain, the Medical Grade (MG) version includes a built in ECG that provides medical grade ECG readings. To take an ECG reading with WHOOP MG, one places their thumb and index finger on the designated sensor indents in the clasp while remaining stationary for 30 seconds. The device then provides a rhythm summary. While WHOOP 5.0 uses PPG for passive tracking the MG option adds ECG capability for users needing on demand, clinical grade heart rhythm analysis. This progression further supports WHOOP's overarching goal of contributing to user's health care ecosystem through accurate, real time physiological data.
As WHOOP founder Will Ahmed mentions, “WHOOP was founded on strain and recovery.” A frequent, consistently mentioned critique pertains to the design choice and absence of a screen. However, as Ahmed mentions, this was a decision rooted in the company's focus solely on functionality. Ahmed further emphasized the importance of avoiding "scope creep," and deliberately steering clear of features like push notifications or interactive displays that could shift WHOOP from a performance focused wearable into the broader category of smartwatches. This intentional design ensures that the device remains centered on physiological monitoring rather than digital distraction. As I've previously mentioned in my article "The Longevity Myth: Revisited" an AI driven ecosystem, implementing one's entire data, prioritizing prevention, fully integrated into one's healthcare network is a near future reality. WHOOP not only provides the capability, but also the desire to be an integral player in this advancement.
Blood glucose dysregulation is a major global health concern, affecting an estimated 1 in 5 individuals (approximately 1.2 billion people) who are either prediabetic (~635 million), living with Type 2 diabetes (~550 million) or managing Type 1 diabetes (~9 million). Importantly, diabetes manifests in different forms. An autoimmune condition, Type 1 diabetes destroys pancreatic β-cells, resulting in absolute insulin deficiency and requiring lifelong exogenous insulin therapy. In contrast, Type 2 diabetes is primarily characterized by insulin resistance and relative insulin deficiency, where the body produces insulin but fails to utilize it effectively. Regardless of type, continuous glucose monitoring (CGM) provides valuable real time data, enabling individuals to make timely lifestyle or therapeutic decisions to both manage current disease and may enable earlier detection of dysregulation and guide preventative strategies in at risk individuals.
Historically, glucose regulation has been primarily assessed through hemoglobin A1C, a marker that reflects average blood glucose levels over the preceding two to three months. According to the American Diabetes Association (ADA), A1C levels below 5.7% are considered within the normal, non-diabetic range; levels between 5.7% and 6.4% indicate prediabetes; and levels at or above 6.5% meet the diagnostic criteria for diabetes. Notably, research has shown that individuals with A1C levels at the lower end of the normal range may experience additional health benefits, including a reduced risk of all-cause mortality, regardless of diabetic status. While widely accepted, A1C testing has limitations due to its dependence on red blood cell lifespan and turnover. Conditions like anemia or hemoglobin disorders can distort results and may not accurately reflect true glycemic control.
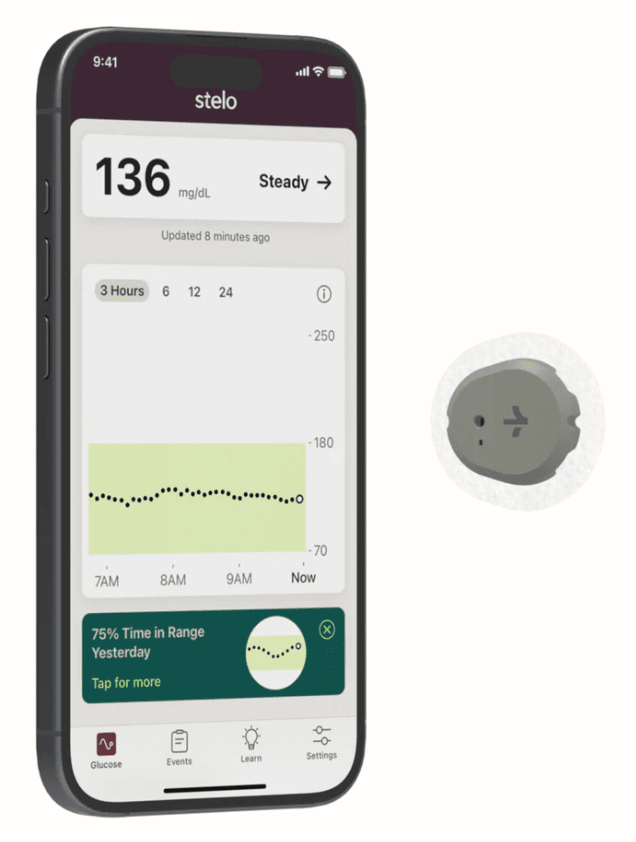
Continuous glucose monitors (CGMs), once reserved primarily for individuals managing Type 1 or Type 2 diabetes, are gaining traction and popularity among broader health conscious consumers. This shift is fueled by the growing interest in preventive health tools, offering real time data and personalized insights that inform lifestyle and dietary decisions. With continuous access to glucose levels, users can observe how specific foods, meal timing, sleep quality and physical activity affect their blood glucose responses, providing actionable feedback rooted in quantifiable metabolic trends.
Outside of traditional clinical settings, CGMs are also proving valuable for personalized nutrition. Interestingly, variability in glucose response to identical meals highlights individual differences in insulin sensitivity, gut microbiota and metabolic health. This real time feedback reinforces behavioral change by emphasizing the effects of lifestyle factors such as exercise, stress and sleep on glucose regulation. Minimal effort behavioral strategies, such as walking post meal, can enhance glucose uptake by activating GLUT-4 transporters in skeletal muscle, the body’s largest glucose sink. These insights compliment other health and wellness tools and strategies to further enable users to tailor their habits and support long term metabolic resilience amid the growing prevalence of prediabetes.
CGMs operate by inserting a small sensor into the subcutaneous tissue, where it samples glucose levels from the interstitial fluid rather than directly from the bloodstream. Although the sensor measures glucose in interstitial fluid, numerous studies have demonstrated that interstitial glucose concentrations closely correlate with blood glucose, particularly when tracking trends over time. Although interstitial values can lag blood glucose by approximately 5 - 15 minutes, the overall accuracy and reliability to assess the dynamic patterns of CGMs are well established. Being a validated, valuable tool for behavioral feedback and metabolic tracking has led to their widespread acceptance for glycemic monitoring and management.
CGMs offer three additional, easily interpretable feedback metrics that provide insight into one's metabolic health. First is the time it takes for blood glucose levels to return to baseline following a meal (typically within 90 to 120 minutes). A prolonged return to baseline may indicate impaired glucose tolerance or insulin resistance, both of which are established early markers of metabolic dysfunction. Notably, the area under the glucose curve (AUC) following food intake reflects the total glycemic exposure with a lower AUC is generally favorable, while an elevated AUC is associated with reduced insulin sensitivity. CGMs can reveal transient fluctuations in insulin sensitivity influenced by lifestyle factors such as stress, sleep deprivation or illness. These dynamic insights allow users to recognize how day to day behaviors affect glucose regulation in real time.
Another key metric to monitor is glycemic variability, or the degree to which blood glucose levels fluctuate throughout the day. Elevated glycemic variability is increasingly recognized as an indicator of underlying metabolic dysfunction and may be associated with oxidative stress, endothelial damage or poor glycemic control. Low variability, referred to as “time in range,” is considered optimal. Although minor fluctuations are normal, particularly in response to meals or physical activity, consistent spikes and crashes are more typical of individuals consuming a standard American diet. Intentional lifestyle choices such as postprandial walking may blunt some of these rises in glucoses; however, achieving sustained low variability often requires a comprehensive and personalized approach to nutrition, exercise, sleep and stress management.
The third metric is the dawn effect which refers to a natural rise in blood glucose caused by the rise in hormones such as cortisol, growth hormone, glucagon and epinephrine during the early morning hours, stimulating hepatic glucose output and temporarily reducing insulin sensitivity. This effect is most pronounced in individuals with Type 1 or Type 2 diabetes, whose impaired insulin response prevents adequate regulation of the increase in blood glucose. On a CGM, the dawn effect typically appears as a gradual, early morning glucose increase independent of food intake. Recognizing this pattern is essential for optimizing medication timing, adjusting nutritional strategies and refining lifestyle interventions to support more stable morning glycemic control. While a dawn effect glucose rise in non-diabetic individuals is not definitively linked to insulin resistance, exaggerated or poorly regulated elevations may reflect early metabolic dysregulation and warrant closer monitoring.

Perhaps the most recognizable consumer health wearable is the Apple Watch. This watch integrates multiple validated sensing technologies into a wearable designed to monitor a wide range of health metrics with additional focus on fashion. It uses PPG to measure HR and HRV, particularly during sleep, while a single-lead electrocardiogram (ECG) enables the detection of cardiac rhythms such as atrial fibrillation and sinus rhythm. The ECG feature, which mimics Lead I in clinical ECGs, is FDA-cleared as a Class II medical device and considered medical grade for specific rhythm assessments though it does not replace a full 12-lead ECG and may be limited by motion artifacts and skin contact issues. Additional sensors include red and infrared LEDs for blood oxygen monitoring, an accelerometer, gyroscope, GPS, barometric altimeter, and skin temperature sensor, supporting the tracking of sleep, activity, elevation, ovulation trends and even early signs of illness. While not a substitute for clinical diagnostics, the Apple Watch offers scientifically valid insights that, when interpreted with an understanding of its limitations, provide accurate and actionable data for health conscious users wishing to monitor their wellness and fitness in daily life.
The Apple Watch stands out among consumer wearables as a clinically validated, FDA cleared device that provides actionable health insights. Its combination of electrical and optical heart sensors has been validated in peer reviewed studies, demonstrating over 94% sensitivity and specificity in detecting atrial fibrillation. These capabilities elevate it beyond basic fitness trackers, offering meaningful contributions to early risk detection and medical awareness. Notably, Apple’s ecosystem also influences user behavior, a challenging yet crucial objective in preventive health. Features such as stand reminders and activity alerts have been shown to promote physical activity and support behavioral consistency. In alignment with the broader goals of health wearables, the Apple Watch delivers continuous, real time feedback designed to encourage sustained, health promoting lifestyle changes.
At the core of the behavior driven approach lies the Apple Health ecosystem. This centralized platform aggregates data from the Apple Watch, iPhone and additional third part apps. As a health data hub, individuals can continually reference to make personalized, informed decisions. In more severe, less frequent scenarios, one can also become aware of otherwise unseen medical indications leading to early clinical interventions. By converting Apple Watch data and the other platforms one chooses to integrate, insights allow a broad health tool for sustained engagement, preventative awareness and lasting behavior change. This built in ecosystem provides a unique advantage when intending to track trends overtime, especially if pairing your Apple Watch with other health wearables (Oura Ring) for a targeted, additional aspect of your health monitoring plan.
The current landscape of health wearables reflects a rapid evolution in consumer grade physiological monitoring. These devices integrate increasingly advanced sensors to track key physiological metrics. While not replacements for clinical diagnostics, they offer validated, actionable insights that can support behavior change, optimize training and recovery and encourage early detection of physiological imbalances. Ultimately, the effectiveness of any wearable lies in its alignment with the user’s personal health goals. By thoughtfully selecting devices based on specific priorities, you can build a tailored toolkit that informs smarter decisions. As sensor technologies become more seamless and multi-analyte platforms emerge, the future of health tech will likely be defined by personalized, data driven health ecosystems that empower users with meaningful, real time insight into their own biology.
The ongoing advancement of wearable technology is moving toward this integrated, data-driven healthcare ecosystem. As sensors become more precise and capable of measuring multiple biomarkers simultaneously, these devices will increasingly serve as valuable tools within personalized healthcare practices. Future wearables will seamlessly communicate with clinical systems, enabling continuous monitoring that supports early intervention and tailored treatment plans. This evolution will empower both users and healthcare providers with real time with actionable insights enabling consumer grade wearables to contribute meaningfully to preventative care, chronic disease management and overall wellness optimization. This interconnected approach will transform how we prevent, manage and optimize health in everyday life.



