The Supplement Playbook: The Science of Strategic Supplementation

When it comes to optimizing health, preventing chronic disease and supporting performance, supplements can play a complementary role alongside foundational nutrition, exercise and lifestyle strategies. While supplements are not meant to be substitutes for whole foods, they have consistently demonstrated benefits in clinical research and can provide noticeable improvements to one's health and performance. Below are five well studied options that form a strong foundation, intended to be additive to a solid diet and exercise plan, for one's overall health and well-being.
Before adding any supplement to a regimen, it’s essential to approach the decision with precision and intent. Begin by clarifying whether the objective is to correct a deficiency or pursue optimization, and whether the ultimate aim is to enhance health span, extend lifespan or both. This clarity allows for more deliberate, consistent strategies aligned with measurable outcomes. Additionally, each supplement should have a measurable biomarker (or known proxy) to track progress and a clearly understood mechanism that can be explained or easily understood. Most importantly, the potential benefit must meaningfully outweigh any associated, known risk to ensure every selection is grounded in evidence, clarity and purpose.

Vitamin C is a potent antioxidant essential for collagen formation, immune defense and cardiovascular support. It protects cells from oxidative stress, strengthens skin and connective tissue, and contributes to neurotransmitter synthesis influencing mood, cognition and stress resilience. Supplementation has been shown to reduce the duration of the common cold, highlighting its vital (and perhaps most well known) role in immune function.
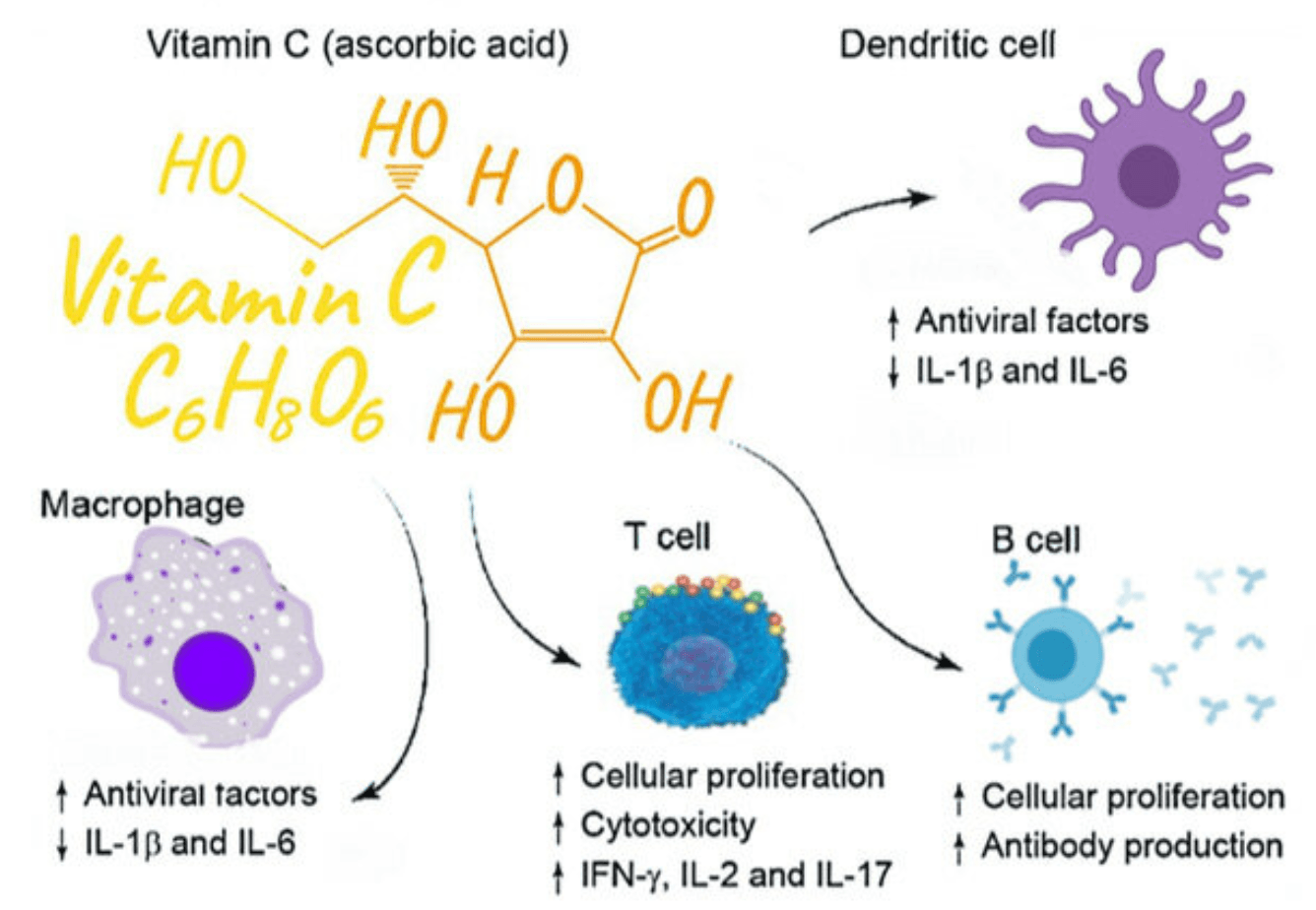
Neutrophils and lymphocytes (endogenous immune cells) have 50–100 times greater vitamin C levels than those found in blood plasma. This targeted adaptation enhances their oxidative burst capacity while simultaneously protecting these cells from oxidative damage. Vitamin C also regenerates other antioxidants such as vitamin E, preserves cellular redox balance, and supports the biosynthesis of carnitine, a molecule essential for mitochondrial energy metabolism during immune activation. It also simlutaneously promotes T cell proliferation and survival, strengthens the adaptive immune response, and modulates cytokine signaling to help maintain inflammatory balance and antiviral defense.
Beyond immunity, vitamin C improves iron absorption from plant based foods and helps buffer oxidative stress from intense exercise, potentially reducing muscle damage, fatigue and post-exercise immune suppression. However, high doses may blunt some of the adaptive benefits driven by reactive oxygen species, suggesting timing and dosage should align with individual goals. When used with intention, vitamin C remains a foundational nutrient for both optimal health and performance resilience.
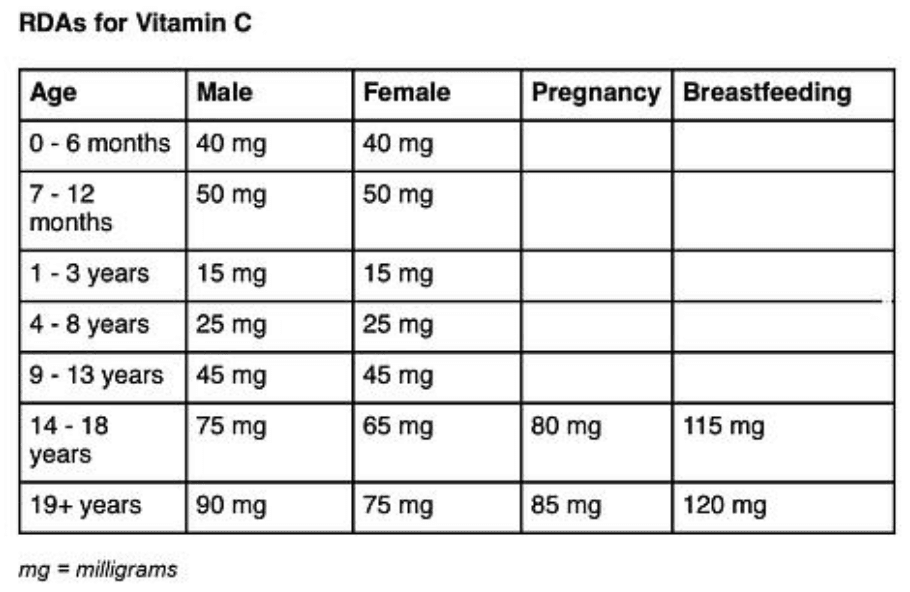
Vitamin C requirements vary by age, sex and life stage, with needs peaking in early adulthood and increasing during pregnancy and breastfeeding. The goal of intake is to achieve plasma levels around 50 µmol/L, supporting the previously mentioned antioxidant protection, immune function, collagen synthesis and overall cellular health. While the recommended dietary allowance (RDA) is designed to meet these needs, the tolerable upper intake limit is 2,000 mg per day primarily to avoid GI discomfort. Even at doses up to 10 grams daily, vitamin C remains well tolerated in healthy adults, though higher doses offer limited additional benefit due to absorption limits. Individuals with elevated iron stores or on iron chelation therapy should limit intake to around 200 mg daily, as higher doses may enhance iron absorption and promote oxidative stress. Concerns regarding kidney stones has surfaced due to vitamin C being metabolized to oxalate, however, sufficient clinical data reveals minimal risk to healthy individuals at dosages below the highest levels. For most individuals, moderate, consistent vitamin C supplementation provides optimal benefits without adverse effects.
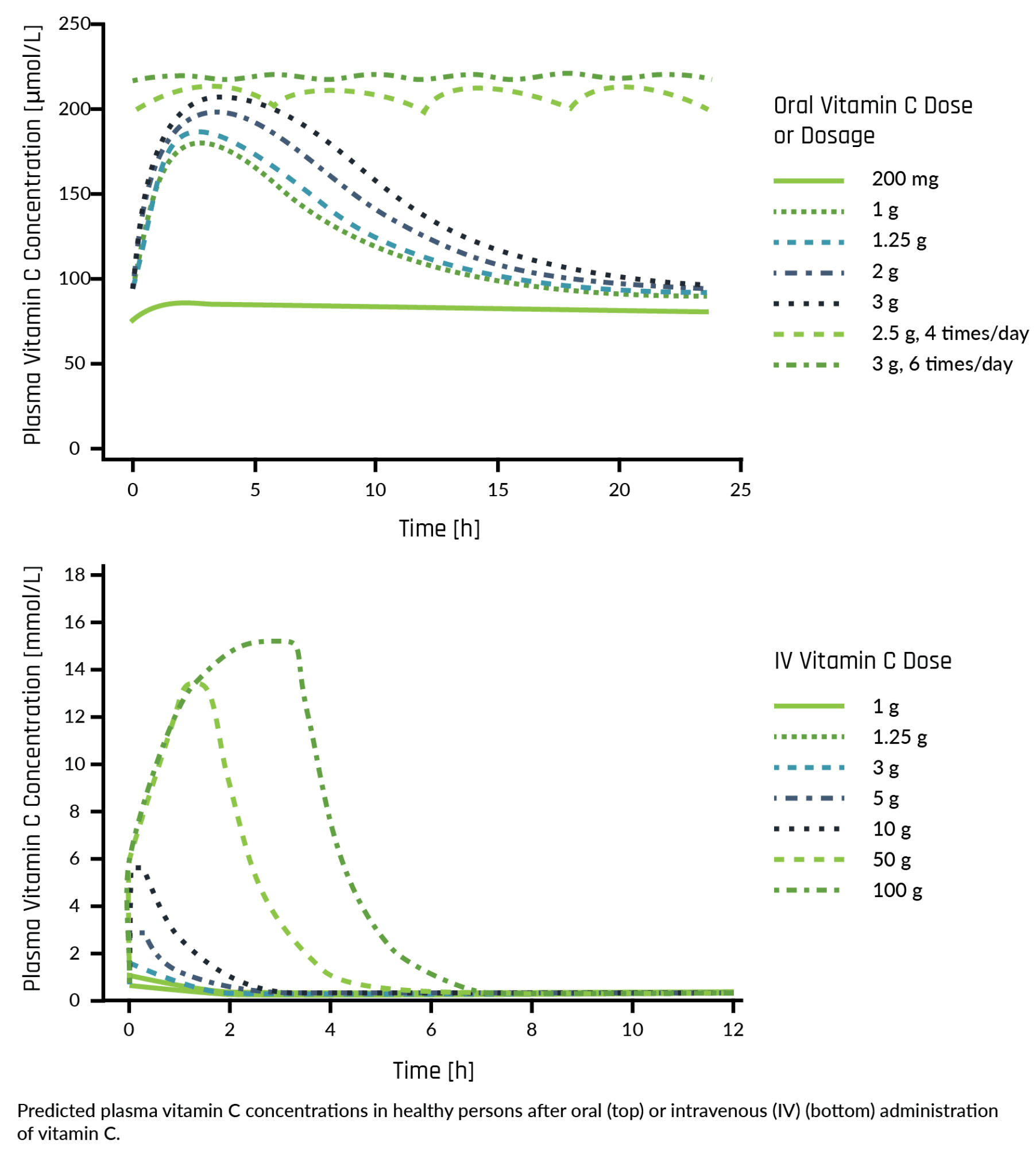
The form of vitamin C you take greatly influences how your body absorbs and utilizes it. Standard oral supplements reach peak plasma concentrations around 70–90 µmol/L before excess amounts are excreted. Liposomal vitamin C can achieve 2 to 3 times higher plasma levels by enhancing cellular uptake and extending circulation time, making it a more efficient option for daily use. For targeted or clinical purposes, intravenous (IV) vitamin C bypasses digestion entirely, achieving millimolar concentrations (1,000–5,000 µmol/L) associated with therapeutic effects on immune function and oxidative stress. Understanding these differences in absorption and bioavailability allows for targeted, evidence-based supplementation tailored to one’s specific health goals. For most individuals seeking immune support or general health benefits, consistent oral intake offers the most practical and effective method of administration. Ultimately, vitamin C exemplifies how a single nutrient can bridge immune defense and systemic performance, leading to measurable positive health outcomes. The evidence highlights vitamin C as one of the most studied and indispensable nutrients in human physiology to support systems that span immunity, cardiovascular health, metabolism and cognition. Its broad biological use cases, clinical versatility and excellent safety profile make it a pillar of preventive health and performance optimization.

vitamin D, often called the "sunshine vitamin," is a fat-soluble steroid hormone that regulates calcium and phosphate balance, immune function, cell growth, glucose metabolism and inflammation through the modulation of hundreds of genes. It is synthesized in the skin upon UVB exposure and activated in the liver and kidneys, with cofactors such as magnesium and vitamin D binding protein influencing its activity. Two main forms exist, vitamin D₂ (from plants and fungi) and vitamin D₃ (from sunlight, animal sources and supplements). Vitamin D₃ is more effective at raising and maintaining serum levels, making it the preferred form for supplementation.
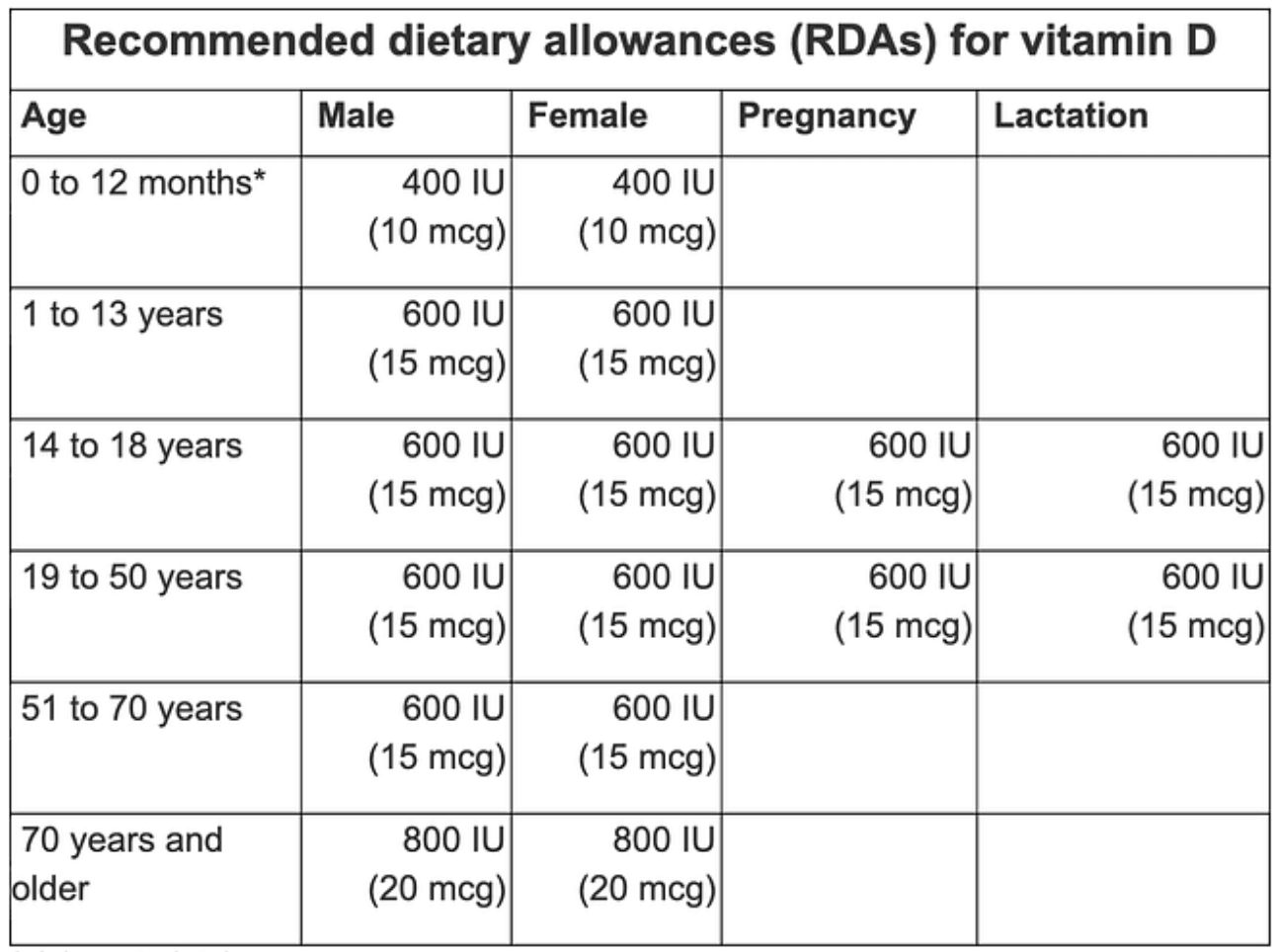
Adequate vitamin D is essential for bone mineralization and strength but also supports cardiovascular, metabolic and immune health, with growing evidence linking it to cognition, mood and healthy aging. Alarmingly, up to 70% of U.S. adults have suboptimal vitamin D levels, with roughly half meeting the criteria for deficiency. Risk prevalence is highest among those with darker skin, obesity, advanced age, chronic illness or limited sun exposure, and aging alone can reduce the skin’s ability to synthesize vitamin D by 50–75%. Deficiency has been associated with osteoporosis, insulin resistance, weakened immunity and greater chronic disease risk. Many experts suggest serum 25-hydroxy vitamin D levels of 40–60 ng/mL considered ideal. For this reason, 50 ng/mL is often the targeted serum level of 25-hydroxy vitamin D (a proxy for vitamin D levels). In practice, supplementation with ~5,000 IU/day of a high quality vitamin D3 supplement is often sufficient to reach this range, though requirements vary by genetics, sun exposure, and co-nutrients such as magnesium levels. Because vitamin D is fat-soluble and accumulates in the body over months, routine blood testing is advised to personalize dosage and ensure safety. Toxic levels typically exceed 150 ng/mL.
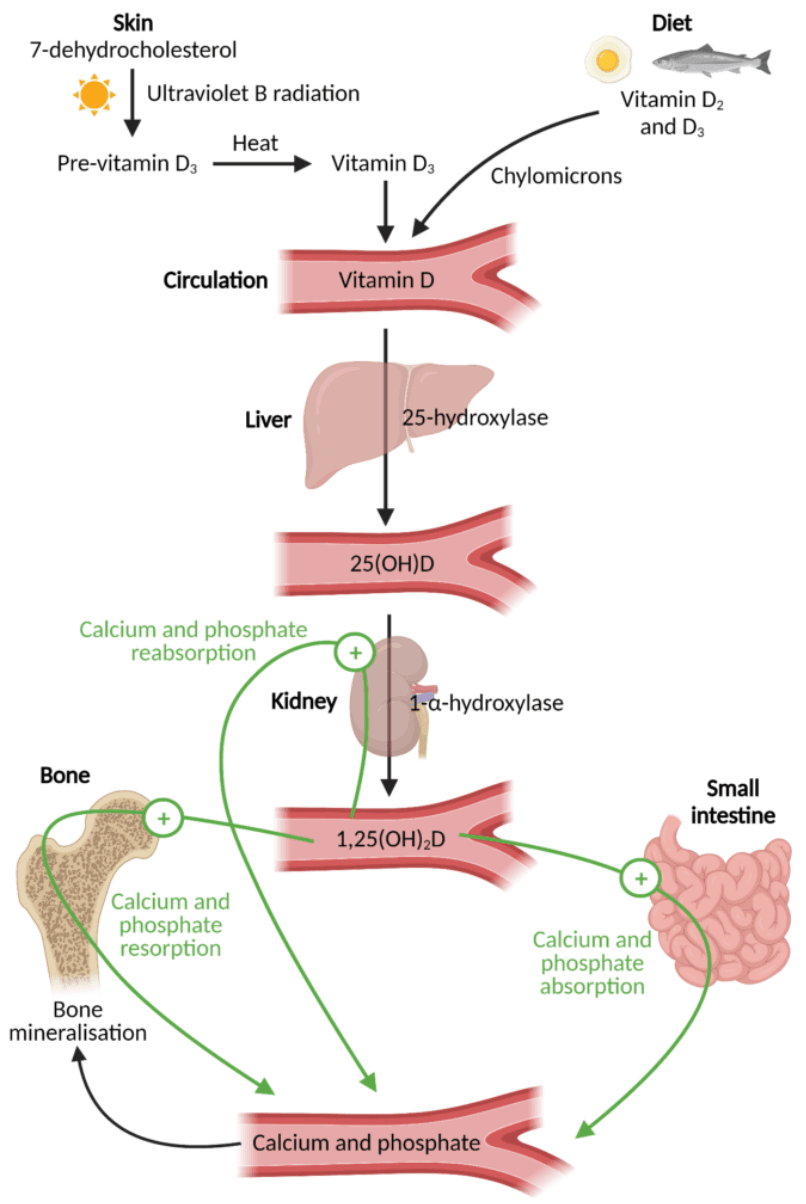
Once produced in the skin or obtained from diet, vitamin D is converted in the liver to 25-hydroxyvitamin D [25(OH)D], the primary circulating form and best indicator of vitamin D status. In the kidneys, it is further activated to 1,25-dihydroxyvitamin D [1,25(OH)₂D], which regulates calcium and phosphate by promoting intestinal absorption, renal reabsorption and bone mineralization. Because 25(OH)D reflects both intake and skin production and has a long half-life, it is the most reliable clinical marker, making adequate levels critical for skeletal health and broader physiological functions. Deficiency disrupts this pathway, leading to reduced calcium absorption, hypocalcemia and compensatory hyperparathyroidism. The resulting symptoms can manifest as rickets in children, osteomalacia in adults and increased osteoporosis risk.

Vitamin D’s effectiveness relies heavily on its interaction with other key nutrients, most notably vitamin K and magnesium. Vitamin D increases production of vitamin K dependent proteins, which help deposit calcium into bones while preventing it from accumulating in arteries. Without sufficient vitamin K, these proteins remain inactive, diminishing bone benefits and raising cardiovascular risk. Similarly, magnesium is essential for activating vitamin D and converting it to its bioactive form yet roughly 50% of U.S. adults are deficient. This further highlights the importance of comprehensive, routine blood work to ensure intended therapeutic ranges are met and contributing factors are addressed to ensure a holistic, comprehensive approach to managing one's health status.
Vitamin D is also stored in body fat, and both weight loss and exercise can enhance vitamin D status by mobilizing these reserves and improving metabolic activation. Studies show that losing about 15% of body weight can nearly triple vitamin D increases compared to smaller losses, while a single 60 minute workout can transiently raise circulating 25(OH)D by roughly 10% and its active form by up to 35%. Regular exercise, especially during low sunlight months, can help maintain active vitamin D levels and reduce seasonal declines, suggesting that movement itself enhances vitamin D metabolism in ways supplementation alone cannot.

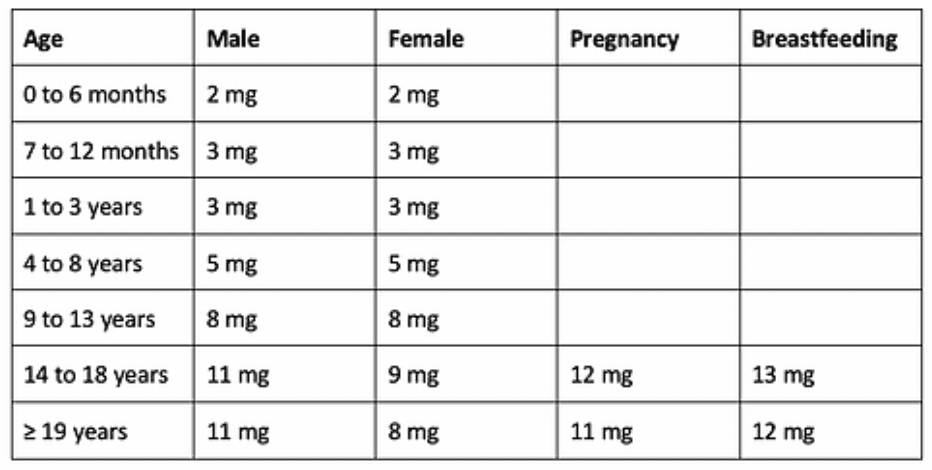
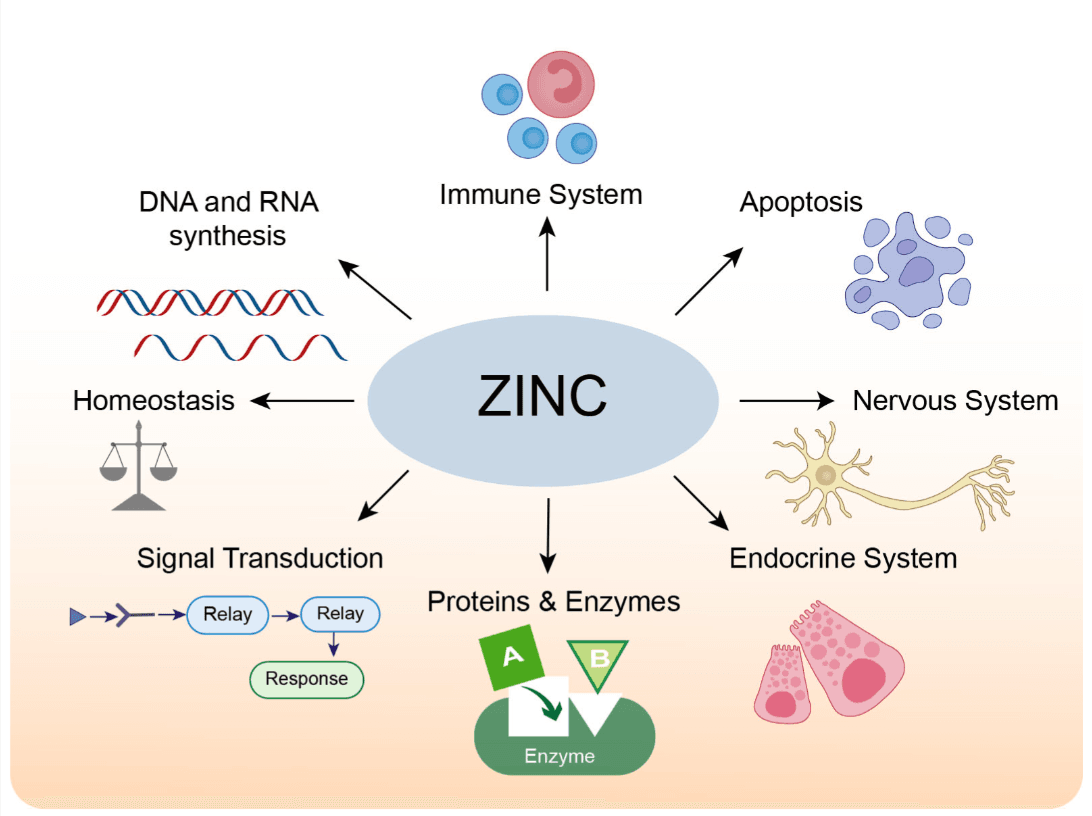
Zinc is an essential trace mineral required for over 300 enzymatic reactions and the regulation of more than 2,000 transcription factors, making it integral to nearly every major biological system. It supports immune defense, DNA and protein synthesis, cell division, wound healing and reproductive health. Even mild deficiency can impair immunity, slow recovery and disrupt metabolic balance. Clinical trials show that zinc lozenges can shorten the duration of the common cold, and the mineral also contributes to taste perception, glucose regulation and hormonal balance.
The body contains roughly 2–3 grams of zinc, primarily stored in skeletal muscle (~60%) and bone (~30%), with less than 0.1% circulating in serum. Absorption averages around 30–35% from mixed diets but can fall to 20% in the presence of phytates from grains and legumes. Zinc is most abundant in oysters, beef, poultry, and shellfish, while plant-based sources provide smaller, less bioavailable amounts. The average U.S. intake is roughly 12 mg daily. In children, deficiency contributes to growth impairment and increased infection risk, while supplementation of 5–15 mg daily has been shown to improve growth and reduces illness duration and mortality in malnourished populations. Vomiting is the most common side effect of excessive intake.
Assessing zinc status is challenging due to tight homeostatic regulation and daily serum fluctuations. Serum zinc (70–100 µg/dL) remains the standard biomarker but can vary by up to 20% in a single day and responds modestly to short term dietary changes. Zinc levels found in the hair offer a view of long term status, while urinary zinc reflects total body stores, though both have limitations. Emerging biomarkers, including zinc dependent enzymes involved in fatty acid metabolism, may provide more precise assessment in the future. For most individuals, consistent dietary intake and moderate supplementation are sufficient, with blood monitoring every 6–12 months recommended for those at risk or using higher dose regimens.
Importantly, zinc is central to immune defense. By supporting T cell development via the zinc-dependent hormone thymulin, Zinc protects neutrophils and macrophages from oxidative stress to elicit direct antimicrobial effects. It inhibits replication of RNA viruses through RNA polymerase blockade (a process enhanced by the above mentioned ionophores) and modulates inflammation to maintain immune balance and prevent tissue damage. These mechanisms further highlight zinc’s dual role as both immune activator and regulator, essential for balanced defense and recovery.
Supplemental effectiveness depends largely on the zinc form. Common types include gluconate, citrate, picolinate, acetate, and sulfate. Comparative studies suggest zinc citrate and gluconate have the highest bioavailability (~60%), while zinc oxide performs less efficiently (~50%). Zinc picolinate may increase red blood cell and hair zinc levels but also elevates urinary loss, suggesting reduced long term retention. Clinically, both zinc acetate and zinc gluconate lozenges can reduce cold duration at doses of 80–100 mg per day, indicating that total elemental intake may matter more than compound type for short term immune support. Supplements in the form of capsules and tablets remain practical for daily preventive use and can be made even more effective when paired with natural ionophores like quercetin or polyphenols, which help enhance antiviral activity against viruses.
Zinc absorption is optimal on an empty stomach but may be taken with food to minimize GI discomfort. Minerals such as iron and calcium, and compounds like phytates, can reduce absorption efficiency. For most individuals, zinc citrate and zinc gluconate provide the best balance between efficacy, tolerability and safety to support immune resilience, recovery and metabolic function when taken consistently within recommended limits. Chronic intake above 50 mg per day can disrupt copper and iron balance, suppress immunity and has been linked to increased prostate cancer risk. As with all supplementation, the key is precision paired with adequate, but not excessive intake, guided by diet, physiology and periodic monitoring.

Magnesium functions as a cofactor in more than 300 enzymatic reactions, influencing calcium and potassium balance, glucose metabolism, bone formation and neuromuscular signaling. Approximately 60% of total body magnesium is stored in bone, where it supports mineral structure and regulates the balance between bone formation and resorption. Adequate magnesium levels are essential for insulin sensitivity, carbohydrate oxidation and the regulation of nerve and muscle activity. Deficiency is associated with muscle cramps, fatigue, mood changes, migraines, arrhythmias and low bone density. Common contributors include low dietary intake, certain medications (PPIs and diuretics), gastrointestinal disorders and alcohol use.
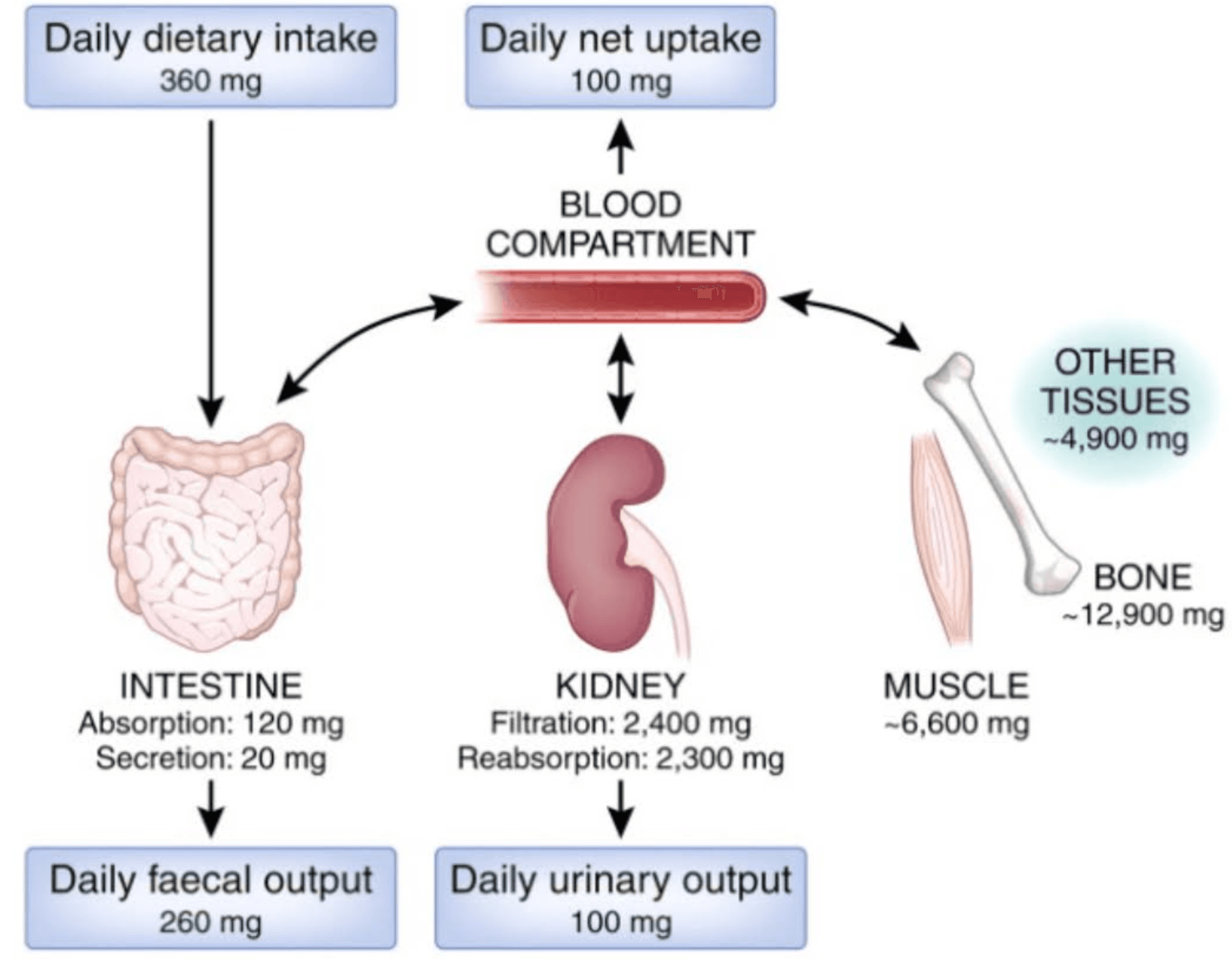
Assessing true magnesium status is challenging because only about 1% of total body magnesium circulates in the blood, meaning serum levels often fail to reflect intracellular or total body stores. More precise methods such as 24 hour urinary magnesium excretion or magnesium retention testing after intravenous loading can reveal insufficiency or deficiency. However, these tests are rarely performed outside of specialized clinical or research settings due to cost and complexity. As a result, magnesium deficiency is frequently under diagnosed, and physician judgment often guides treatment decisions. Fortunately, in individuals with normal kidney function, magnesium homeostasis is tightly regulated by renal excretion, making deficiency far more common than toxicity. Because mild insufficiency is widespread and current measurement tools are imperfect, clinical practice often favors supplementation when symptoms such as muscle cramps, arrhythmias, or general fatigue are present, even without formal testing. In these cases, supplementation is both safe and effective at supporting cellular energy production, neuromuscular function and overall physiological health.
Most adults consume well below the recommended 420 mg (men) or 320 mg (women) per day, with average U.S. intake around 250 mg. Optimal intake may be closer to 400–600 mg, with higher needs in individuals prone to migraines, alcohol use or increased perspiration. Magnesium is found in nuts, seeds, leafy greens, beans, and dark chocolate, though processing often limits content and absorption. Given its low cost, safety profile and widespread insufficiency, supplementation is a low risk, high reward strategy for health and performance. Clinical evidence supports magnesium supplementation for migraine relief, improved sleep in older adults and potential cognitive benefits, while the main risk in healthy adults is GI discomfort.
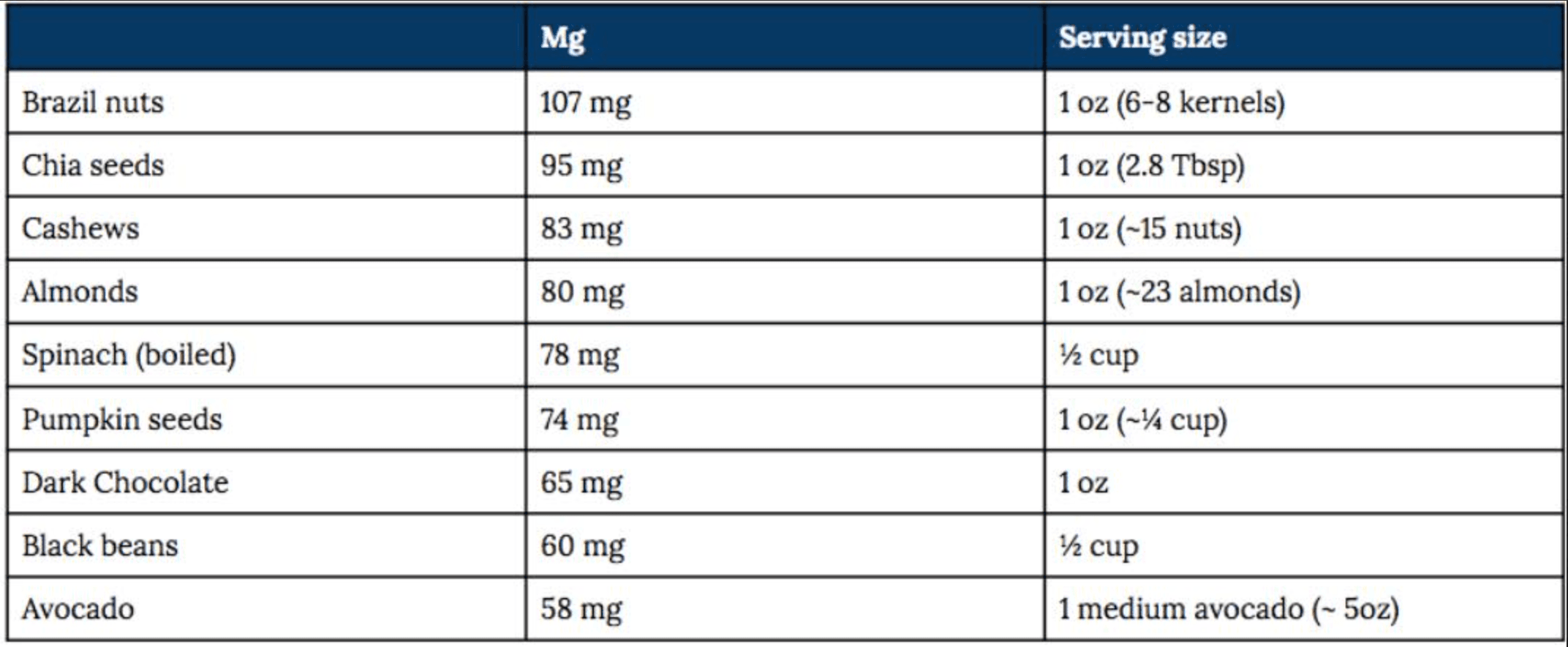
Magnesium supplements differ in absorption and physiological effect, and selecting the right form depends on the intended purpose. They are generally categorized as inorganic salts (oxide, chloride) or organic chelates (glycinate, citrate, malate, lactate, L-threonate). Inorganic forms vary in bioavailability. Magnesium chloride is well absorbed for systemic repletion, while oxide (<10% absorption) is effective primarily for bowel regulation. Organic forms are more efficiently absorbed and preferred for improving total body magnesium status, supporting neuromuscular and metabolic function and managing mild deficiency. Magnesium L-threonate uniquely crosses the blood brain barrier, showing promise for cognitive and sleep benefits, though evidence remains mostly preclinical or from small human studies. Absorption efficiency ranges by form with oxide <10%, citrate ~30–40% and glycinate ~25–50% To ensure intake is fully optimized, it is recommended one takes smaller, more frequent dosages throughout the day.
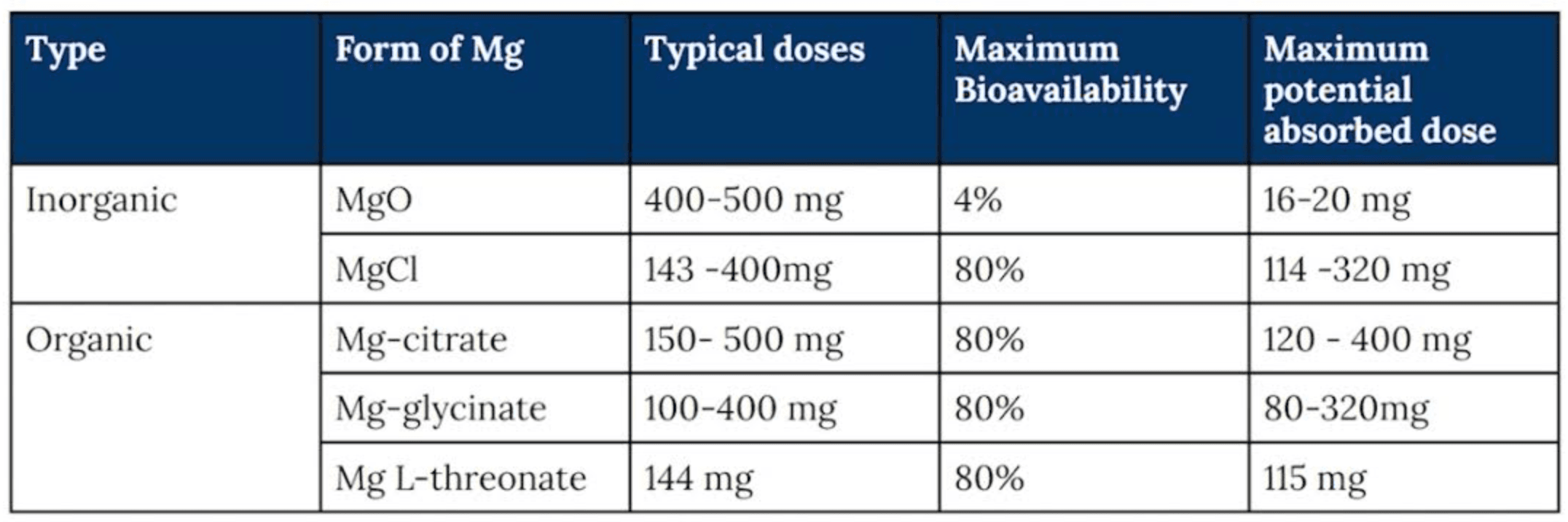
Individual magnesium requirements vary based on diet, physiology and kidney function, but a combined daily intake of 500–600 mg from food and supplementation is generally sufficient for most healthy adults. Magnesium homeostasis is tightly regulated through renal excretion, so supplementation is typically safe in those with normal kidney function, provided doses are divided and tolerance is monitored. Overall, maintaining adequate magnesium intake supports a wide range of physiological processes, including neuromuscular function, energy metabolism, bone health and cardiovascular stability, making it a foundational nutrient for both general health and performance.

Fish oil, rich in EPA and DHA, provides anti-inflammatory benefits that support cardiovascular, metabolic, brain and joint health. Clinical trials consistently show that omega-3s lower triglycerides, reduce systemic inflammation and improve cognitive function, mood regulation and arrhythmia prevention. By promoting the production of specialized pro-resolving mediators and modulating genes involved in immune signaling, omega-3s help regulate inflammation and enhance cardiovascular, cognitive and musculoskeletal resilience.
Mechanistically, omega-3 fatty acids exert their effects by shifting production toward EPA-derived mediators and away from pro-inflammatory compounds. This biochemical shift reduces systemic inflammation and improves endothelial function through nitric oxide signaling while lowering triglycerides and thrombosis risk. These pathways reveal omega-3s’ protective roles in cardiovascular and cancer prevention, decreasing cell proliferation, enhancing apoptosis and limiting angiogenesis. Collectively, these effects demonstrate how omega-3s translate cellular level regulation into broad, clinically measurable health benefits.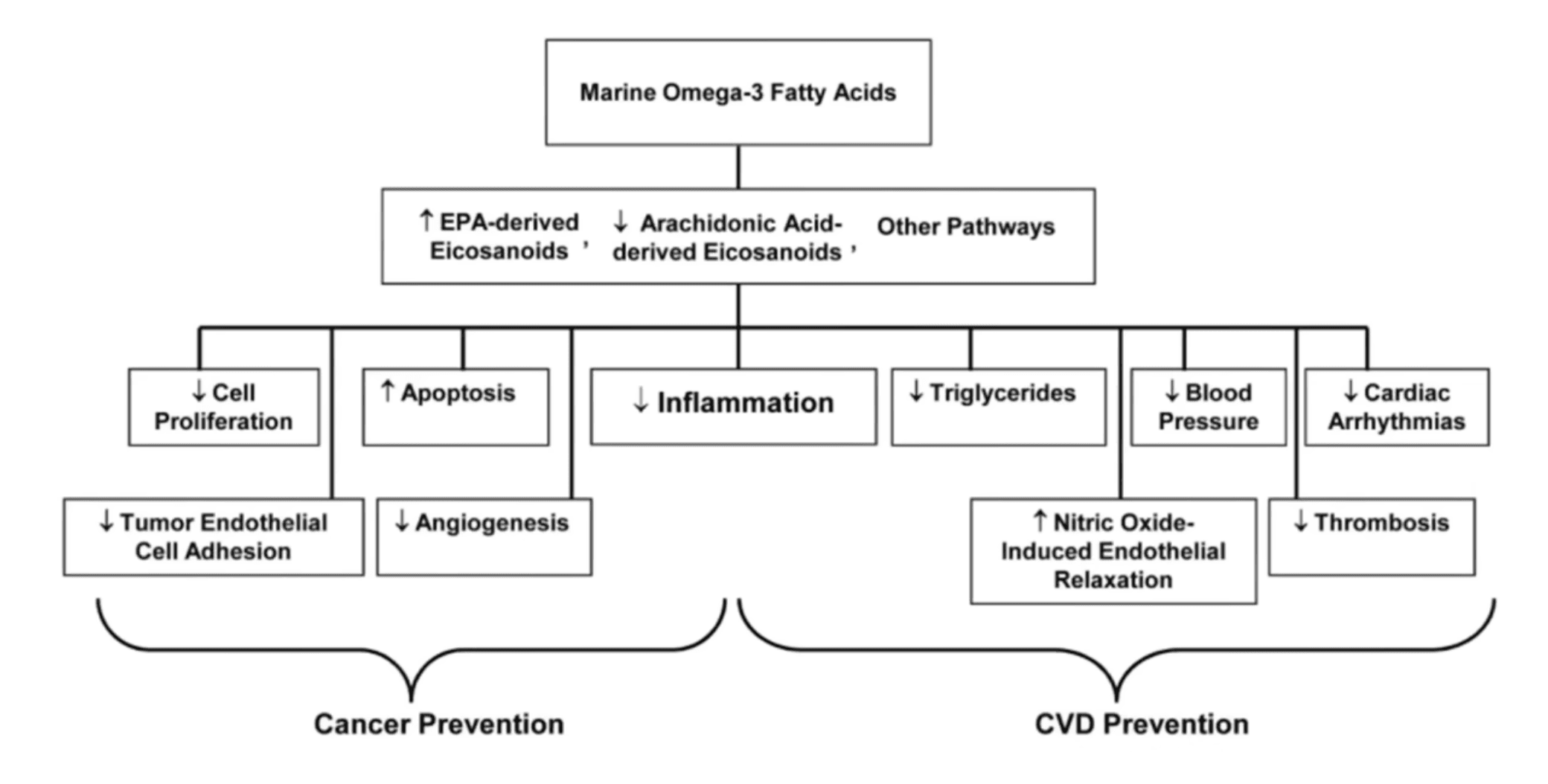
Current dietary guidelines likely underestimate omega-3 requirements. The body converts less than 10% of plant based alpha-linolenic acid (ALA) into EPA and DHA, highlighting the importance of direct intake from fish and high quality supplements such as wild caught salmon, sardines or fish oil. A simple, easily remembered acronym when making high quality sea food selections is SMASH. Salmon, mackerel, albacore tuna, sardines and herring are among the highest quality EPA and DHA containing selections. Achieving an optimal omega-3 index typically requires around 2 grams per day of combined EPA and DHA. Absorption and tissue uptake depend on supplement formulation, baseline omega-3 status, meal composition and genetics. Triglyceride and phospholipid forms are generally more bioavailable than ethyl esters, which require additional digestion and are best taken with a fat containing meal.
The omega-3 index measures the proportion of EPA and DHA in red blood cell membranes and is the most reliable indicator of long term omega-3 status and cardiovascular risk. Because red blood cells live about 120 days, the omega-3 index reflects roughly three months of dietary intake and tissue incorporation. This makes it far more stable than plasma phospholipid levels, which fluctuate based on recent meals or supplements. Similar to my prior article's mention of HbA1C relative to an oral glucose tolerance test, the omega-3 index gives a more accurate, longer term view of one's true omega-3 status. An omega-3 index above 8% is associated with optimal cardiovascular and cognitive outcomes, while values below 4% correlate with higher inflammation, cardiovascular risk and premature mortality. As Dr. William Harris mentions, roughly 90-95% of the US adult population falls below the 8% target range, with the average likely falling around 5.0 - 5.2%.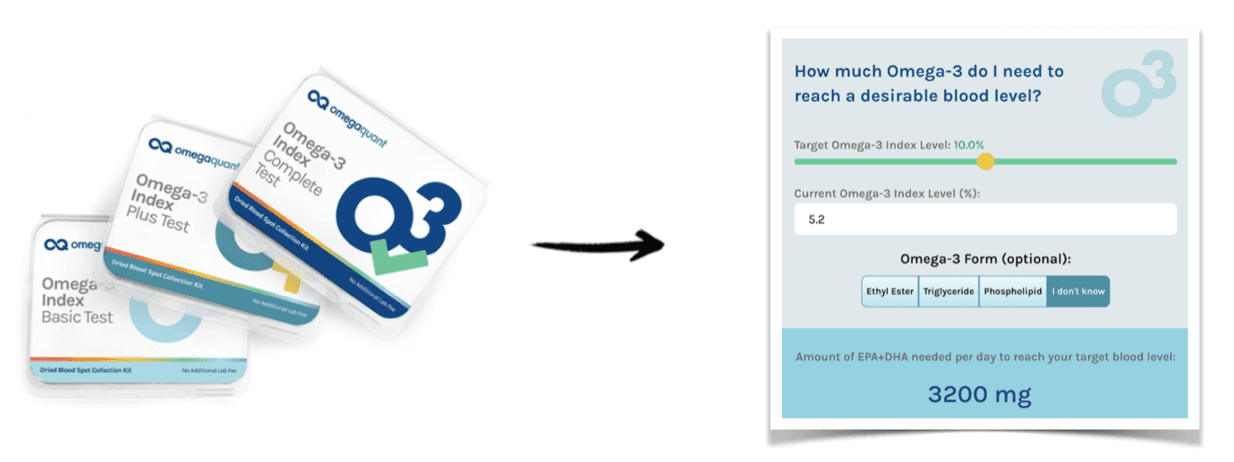
Omega-3 concentrations vary widely between individuals and populations due to genetics, diet, age and sex. Populations with high fish consumption, such as those in Japan or Northern Europe, consistently show higher omega-3 index scores and correspondingly lower rates of cardiovascular disease. Women often maintain higher DHA levels, likely reflecting hormonal and reproductive demands, which further highlights the biological variability in omega-3 metabolism and function. Importantly, higher omega-3 status is strongly associated with reduced cardiovascular risk and all-cause mortality. Clinical trials using purified EPA demonstrate that a daily dose of 4 grams can lower major cardiovascular events by roughly 25% in individuals with elevated triglycerides despite statin therapy. These benefits extend beyond lipid lowering, reflecting anti-inflammatory, antithrombotic and membrane stabilizing effects. Together, these findings highlight the omega-3 index as a clinically meaningful biomarker linking genetics, diet and supplementation to systemic and cardiovascular health outcomes.

Beyond cardiovascular protection, omega-3s support critical effects within the central nervous system. In the brain, DHA supports neuronal growth, synaptic plasticity and white matter integrity, while EPA and DHA together mitigate neuroinflammation and oxidative stress. These mechanisms have been linked to reduced symptoms of depression and slower cognitive decline across multiple longitudinal studies. Notably, individuals with genetic polymorphisms such as APOE4 may require higher or phospholipid rich supplements to achieve comparable brain uptake, further highlighting the importance of personalized omega-3 strategies in cognitive health.
Omega-3 fatty acids also play a critical role in maintaining muscle mass and function, extending beyond their well established cardiovascular and cognitive benefits. Supplementation of approximately 2–5 grams per day has been shown to enhance muscle protein synthesis, improve anabolic sensitivity and reduce muscle loss during inactivity or aging. These effects are especially relevant for older adults, where omega-3s can help preserve strength, mobility and overall functional capacity. When combined with resistance or aerobic training, omega-3 supplementation may further boost strength gains, preserve lean mass and modestly reduce blood pressure. This is particularly valuable during recovery from injury or periods of reduced activity.
At the cellular level, omega-3s integrate into muscle cell membranes, enhancing amino acid signaling and mitochondrial efficiency. This improves the anabolic response to dietary protein and reduces inflammation within muscle tissue, counteracting the anabolic resistance that accompanies aging and physical inactivity. By supporting both anabolic signaling and anti-inflammatory pathways, omega-3s act synergistically with exercise to optimize muscle adaptation and recovery. Although evidence for these protective effects is strong, future research should clarify optimal dosing and tissue thresholds necessary to achieve meaningful improvements in muscle function.
Creatine is one of the most extensively studied and well-validated supplements, recognized for its central role in cellular energy metabolism and its broad applications across both physical and cognitive performance. Stored primarily in skeletal muscle and the brain as phosphocreatine, it functions as a rapid energy reserve that regenerates ATP during periods of high demand to support strength, endurance, and mental performance. Beyond its athletic benefits, emerging evidence highlights creatine’s neuroprotective and metabolic effects, suggesting value in cognitive resilience, healthy aging and recovery from stress or injury. Overall, creatine represents a scientifically validated, multifunctional compound with benefits spanning muscle, metabolism and brain health. Those interested in more information on creatine, including its mechanisms, dosing strategies and emerging applications can view my prior article, Creatine: An Emerging Panacea?
As previously referenced, regular biomarker testing is the foundation of any intelligent supplementation strategy. Measuring key nutrients such as zinc, magnesium, vitamin D, vitamin C and the omega-3 index every six months provides objective insight into metabolic balance, nutrient sufficiency and overall physiological function. Without this data, even well intentioned health efforts risk becoming speculative rather than strategic.
Direct to consumer testing platforms have transformed accessibility, offering robust, laboratory grade assessments once limited to clinical research settings. These services allow for precise, high volume analysis of key biomarkers delivered efficiently and often at a fraction of traditional clinical cost. By tracking results over time, individuals can identify subtle deficiencies or imbalances that may affect cognition, energy, immunity and long term health trajectory.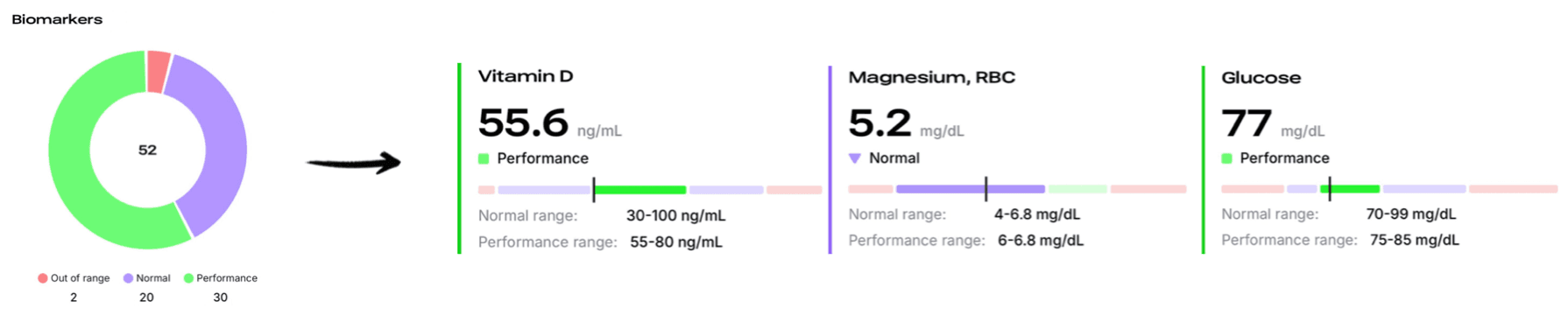
Consistent monitoring replaces guesswork with measurable progress. Many only realize the full benefits of nutrient optimization, including enhanced energy, sharper cognition and improved immune system resilience once deficiencies have been corrected and optimal ranges sustained. Data driven testing is therefore not merely an adjunct to supplementation, but the feedback loop that transforms health optimization into a measurable, personalized science.
In summary, optimal health and performance begin with strong nutritional and lifestyle foundations, but targeted supplementation can further enhance resilience, energy and longevity. The five evidence-based supplements discussed support critical systems including immunity, cardiovascular health, metabolism, cognition and muscle function. When used intentionally and monitored through regular biomarker testing, these nutrients can correct common deficiencies and fine tune physiological performance. Personalized, data-driven supplementation not only bridges dietary gaps but also empowers individuals to move from adequacy to optimization to achieve measurable, lasting improvements in health span and overall vitality.

Bryer, S. C., & Goldfarb, A. H. (2006). Effect of high dose vitamin C supplementation on muscle soreness, damage, function, and oxidative stress to eccentric exercise. Journal of Sports Science and Medicine, 5(2), 71–79.
Braakhuis, A. J. (2012). Effect of vitamin C supplements on physical performance. Current Sports Medicine Reports, 11(4), 180–184. https://doi.org/10.1249/JSR.0b013e31826258ea
Levine, M., Rumsey, S. C., Daruwala, R., Park, J. B., & Wang, Y. (1999). Criteria and recommendations for vitamin C intake. Journal of the American Medical Association, 281(15), 1415–1423. https://doi.org/10.1001/jama.281.15.1415
Carr, A. C., & Maggini, S. (2017). Vitamin C and immune function. Nutrients, 9(11), 1211. https://doi.org/10.3390/nu9111211
Wintergerst, E. S., Maggini, S., & Hornig, D. H. (2006). Immune-enhancing role of vitamin C and zinc and effect on clinical conditions. Annals of Nutrition & Metabolism, 50(2), 85–94. https://doi.org/10.1159/000090495
Mocayar Marón, F. J., Munch, M. M., & Hogas, P. (2021). The role of magnesium in the pathogenesis of metabolic disorders. Nutrients, 13(2), 434. https://doi.org/10.3390/nu13020434
Nielsen, F. H., & Lukaski, H. C. (2006). Update on the relationship between magnesium and exercise. Magnesium Research, 19(3), 180–189. https://doi.org/10.1684/mrh.2006.0009
Sadiq, S., Tabassum, S., Enam, S. A., Liaquat, L., Batool, Z., Madiha, S., Shahzad, S., Sajid, I., & Haider, S. (2021). Neurobehavioral and biochemical effects of magnesium chloride (MgCl₂), magnesium sulphate (MgSO₄), and magnesium-L-threonate (MgT) supplementation in rats: A dose-dependent comparative study. Pakistan Journal of Pharmaceutical Sciences, 34(1), 277–284.
Zhang, C., Li, Y., Fathi, A., Wu, H., Qian, S., Huang, Y., Tang, Y., & Tang, Y. (2016). A Magtein® magnesium L-threonate-based formula improves brain cognitive functions in healthy Chinese adults. Nutrients, 8(6), 385. https://doi.org/10.3390/nu8060385
Lowe, N. M., Fekete, K., & Decsi, T. (2009). Methods of assessment of zinc status in humans: A systematic review. American Journal of Clinical Nutrition, 89(6), 2040S–2051S. https://doi.org/10.3945/ajcn.2009.27230H
Prasad, A. S. (2013). Discovery of human zinc deficiency: Its impact on human health and disease. Advances in Nutrition, 4(2), 176–190. https://doi.org/10.3945/an.112.003210
Hemilä, H. (2011). Zinc lozenges may shorten the duration of colds: A systematic review. Open Respiratory Medicine Journal, 5, 51–58. https://doi.org/10.2174/1874306401105010051
Romero Cabrera, A. J., & Ríos Álvarez, M. L. (2019). Zinc, aging, and immunosenescence: An overview. Pathobiology of Aging & Age-Related Diseases, 9(1), 159–170. https://doi.org/10.1080/20010001.2019.1594175
Siwek, M., Dudek, D., Paul, I. A., Sowa-Kućma, M., Zieba, A., Popik, P., & Nowak, G. (2009). Zinc supplementation augments efficacy of imipramine in treatment-resistant patients: A double blind, placebo-controlled study. Journal of Affective Disorders, 118(1–3), 187–195. https://doi.org/10.1016/j.jad.2009.02.003
Harris, W. S., Tintle, N. L., Imamura, F., Qian, F., Korat, A. V. A., Marklund, M., Djoussé, L., Bassett, J. K., Carmichael, P. H., Chen, T. A., Chien, K. L., Chowdhury, R., Del Gobbo, L. C., Fretts, A. M., Giles, G. G., & others. (2021). Blood n–3 fatty acid levels and total and cause-specific mortality from 17 prospective studies. Nature Communications, 12(1), 2329. https://doi.org/10.1038/s41467-021-22370-2
Witte, A. V., Kerti, L., Hermannstädter, H. M., Fiebach, J. B., Schreiber, S. J., & Flöel, A. (2014). Long-chain omega-3 fatty acids improve brain function and structure in older adults. Cerebral Cortex, 24(11), 3059–3068. https://doi.org/10.1093/cercor/bht163
Harris, W. S., & von Schacky, C. (2004). The Omega-3 Index: A new risk factor for death from coronary heart disease? Preventive Medicine, 39(1), 212–220. https://doi.org/10.1016/j.ypmed.2004.02.030
Bhatt, D. L., Steg, P. G., Miller, M., Brinton, E. A., Jacobson, T. A., Ketchum, S. B., Doyle, R. T. Jr., Juliano, R. A., Jiao, L., Granowitz, C., Tardif, J.-C., & Ballantyne, C. M. (2019). Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. New England Journal of Medicine, 380(1), 11–22. https://doi.org/10.1056/NEJMoa1812792
McGlory, C., Calder, P. C., & Harris, R. A. (2020). The influence of omega-3 fatty acids on skeletal muscle protein turnover in health, disease, and disease. Frontiers in Nutrition, 7, 144. https://doi.org/10.3389/fnut.2020.00144

Chau, Y. S., Bruant, L., & Vega, P. J. (2013). The importance of dose, frequency and duration of vitamin D supplementation for plasma 25-hydroxyvitamin D. Nutrients, 5(10), 4067–4077. https://doi.org/10.3390/nu5104067
Ferrucci, L., Calvani, R., Marzetti, E., Cesari, M., Arosio, B., Carta, G., Volpato, S., Rengo, F., & Cherubini, A. (2023). Targeting the hallmarks of aging with vitamin D: Starting to decode the myth. Nutrients, 15(1), 56. https://doi.org/10.3390/nu15010056
LeBoff, M. S., Chou, S. H., Murata, E. M., Cook, N. R., Mora, S., Buring, J. E., Manson, J. E., & the VITAL Research Group. (2022). Supplemental vitamin D and incident fractures in midlife and older adults. New England Journal of Medicine, 387(4), 299–309. https://doi.org/10.1056/NEJMoa2202106
Remelli, F., Vitali, A., Zurlo, A., & Volpato, S. (2022). The effect of vitamin D supplementation on muscle mass, muscle strength and muscle function in the elderly: A systematic review and meta-analysis. Aging Medicine and Healthcare, 13(2), 42–54. https://doi.org/10.3389/amh.2022.00045
Holick, M. F. (2007). Vitamin D deficiency. New England Journal of Medicine, 357(3), 266–281. https://doi.org/10.1056/NEJMra070553



