Understanding Back Pain

A significant percentage of people will experience substantial back pain at some point in their lives. While not all acute episodes develop into chronic conditions, even short term pain can meaningfully disrupt quality of life. In this article, I will provide an overview of spinal anatomy, common movement patterns and behaviors that contribute to back pain, and evidence based strategies for prevention, management and relief. I will also explore key considerations for those aiming to avoid injury, recover from back related issues, manage intermittent or persistent pain or navigate the complexities of pre- and post-operative care. The insights shared are informed by leading experts in pain science, clinicians and researchers who have dedicated their careers to both academic study and real world application.

The spine is a flexible rod capable of bending and stabilizing as needed. While it allows for flexion, extension, and rotation, it is not designed to serve as a primary mover. Instead, greater ranges of motion and dynamic movement should originate from the ball and socket joints of the hips and shoulders. When individuals lack proper movement education, they often develop inefficient motor patterns, commonly referred to as maladaptive neural engrams, which contribute to poor spinal mechanics. Over time, this can lead to compromised "spine hygiene," a term used to describe habitual movement patterns that place unnecessary strain on the spine and increase the risk of injury.
An important consideration in proper movement mechanics is the relationship between duration and load. A non weight bearing spine can typically tolerate greater cumulative strain over time compared to a spine under load. For example, bending forward to tie one’s shoes is a common, usually painless activity that remains harmless in the absence of injury. However, applying the same movement pattern, paired with significant spinal flexion, to a loaded exercise like the deadlift can dramatically increase compressive forces on the spine, raising the risk of injury. While this may seem like a basic comparison, the same principle applies to many everyday movements and exercises. Load and form both matter, especially when previously engrained movement patterns are transferred from low load to high load scenarios.
An equally important factor in promoting optimal musculoskeletal health is allowing adequate recovery time for positive adaptation to occur. Just as muscle tissue requires an appropriate stressor to stimulate growth and strengthening, the spine and its associated structures (ligaments, tendons and bone) also undergo adaptive remodeling in response to mechanical loading. However, this adaptation is only possible when a sufficient recovery period is in place. When the balance between stress and recovery becomes skewed, favoring excessive load with inadequate rest, maladaptive changes can occur, potentially increasing the risk of dysfunction or injury. This principle applies regardless of injury status, though the ideal stress to recovery ratio can vary significantly depending on an individual’s goals, health status and physical capacity. Given the high prevalence of disc related spine injuries and the potential to trigger a degenerative cascade, this article will primarily focus on disc specific back injuries.

Intervertebral discs are composed of interwoven layers of collagen fibers, and structural damage often results from repetitive mechanical stress or poor movement patterns. In the research setting, the most consistently reproducible injury causing mechanics was attributable to high velocities under compressive forces. Excessive bending, rotation and/or compressive forces in any life style and/or training will likely end in injury if the timeline is long enough. This process accelerates in the absence of adequate recovery protocols, such as sufficient rest. Over time, these repeated loading errors and movement flaws can create microtears in the disc’s annular fibers. As we will discuss later, injury is asymmetrically harmful. Often one does not realize the full spectrum of the degenerative cascade, compensation requirements and decreased quality of life as a result of injury until they find themselves managing one. This further highlights patient empowerment through education and the resulting preventative, rather than corrective, strategies in ones daily life and exercise habits. 
Both the collagen composition and the anatomical shape of the disc influence the overall resilience of the spine. Ovoid shaped discs are generally better suited for repetitive bending and flexibility, while lamicon shaped discs tend to tolerate compressive forces more effectively. Regardless of shape, each disc contains a mixture of different collagen types. On average, approximately 80% of the collagen is Type I and 20% is Type II. The remaining 1–5% consists of a individualized blend of Types III through X, which primarily serve as binding fibers that hold the main collagenous structures together. These binding fibers have a high degree of genetic variability, which partly explains why some individuals may show greater resilience to back pain or injury, even when other factors are constant. While poorly selected exercises, especially those involving repetitive stress strain reversals and cumulative stress concentrations are known to contribute to disc injury, individual variability in collagen composition may influence how well one’s spine tolerates mechanical stresses.

While the shape of the intervertebral disc can influence how it responds to mechanical loads, susceptibility to bulges and herniations depend more on disc health, loading patterns, posture and degeneration than on shape alone. Abnormal disc shapes, including asymmetric or ovoid appearances, may reflect degenerative changes, annular tears or previous injury. An ovoid shaped disc may not cause herniation but can reflect early degeneration or deformation, which may increase susceptibility to bulging or herniation. A common statistic mentioned in the medical field is the percentage chance of recurring injury, specifically for those post surgical intervention. While 10% chance of injury is typically mentioned, clinical practice statistics suggests as high as 37% of individuals who've had surgery suffer additional injury to the same level. This is likely multifaceted as to why the prevalence of injury is this high including lack of movement education, exercise modification and unappreciated spinal anatomy differences.

Pain associated with disc injury typically begins when disc material bulges or herniates, impinging on nearby nerve roots. Notably, these displacements are often only a matter of millimeters and in some individuals, as little as 2–3 mm of protrusion can cause significant pain, while others may experience little to no discomfort even with displacements of 8–10 mm. This variability highlights a crucial concept: pain perception is highly individualized, influenced by numerous physiological, neurological and psychological factors, a fascinatingly complex topic that will be explored further in shortly.

Rene Decarte's dualistic biomechanical model of pain
The International Association for the Study of Pain (IASP) defines pain as an unpleasant sensory or emotional experience associated with actual or potential tissue damage." A complex perceptual phenomenon, pain is influenced by factors such as emotional state, context, prior experiences and CNS modulation. Nociceptors are specialized sensory nerve endings that detect potentially harmful stimuli and play a central role in the sensation of pain. Nociceptors convert various forms of stimuli (mechanical, thermal, or chemical energy) into electrochemical signals. These signals are then transmitted as action potentials through two primary types of nerve fibers. Unmyelinated C fibers conduct impulses slowly, at approximately 1 meter per second, and are typically associated with dull, aching, or burning pain. In contrast, A-delta fibers are thinly myelinated and transmit signals much more rapidly, up to 10x faster, resulting in sharp, localized pain sensations. Importantly, the presence and intensity of nociceptive input do not always correlate with the subjective experience of pain.
Chronic pain is pain that persists beyond the expected tissue healing time (typically 3 months) and affects an estimated 50 to 100 million Americans. This broad range is largely attributable to differences in how survey questions are framed with more inclusive definitions of pain tending to yield higher prevalence rates. Regardless of the methodology, the numbers remain alarmingly high. Within this population, approximately 20 million individuals (or about 18%) experience high impact chronic pain (HICP), which is defined as pain that significantly limits daily activities and quality of life. Among those with HICP, lower back pain is the most commonly reported condition, affecting approximately 28% of this group. Additionally, around 16% report chronic neck pain and headaches as contributing factors.

The gate theory of pain
As a multifaceted experience, pain can be broadly classified into several categories based on its origin and underlying mechanisms. Nociceptive pain arises from the activation of nociceptors in response to acute tissue injury and is typically localized and transient. Visceral pain originates from the internal organs, tends to be diffuse and poorly localized and results from the activation of visceral nociceptors. Additionally, neuropathic pain is commonly the result of an acute injury or dysfunction within the peripheral or CNS and is often described as burning, shooting or shock like in nature. The commonly reported "sciatic" pain is a form of neuropathic pain. Finally, and more recently, the concept of nociplastic pain has emerged, referring to pain arising from altered nociceptive processing without clear evidence of tissue damage or disease in the somatosensory system. This classification emphasizes the complexity of pain and the limitations of purely structural explanations.

The biopsychosocial model of pain
When taking a broad view of therapeutic approaches to pain management, one fundamental question arises: is a more favorable outcome achieved by addressing the underlying cause of pain or by focusing on symptom relief? Given the wide range of contributing factors, their complex interplay, and the highly individualized definition of “success,” it becomes clear how challenging prevention, management and potential treatment can be for physiotherapists, pain specialists and surgeons. Aside from the desired level of a health care network one hopes to have access to, chronic pain imposes a significant financial burden on both individuals and society. The total economic cost is estimated to exceed half a trillion dollars annually when accounting for all contributing factors, a figure that surpasses the combined costs of diabetes, heart disease and cancer. As a multifaceted and persistent health concern, chronic pain demands both clinical excellence and systems level coordination and efficiency. While the standard of care is a key driver of outcomes, access to informed healthcare networks, patient education and early awareness often become the limiting factors in effectively initiating and sustaining successful treatment strategies.
Dr. Stuart McGill is a globally recognized spine biomechanist and leading authority on back pain assessment, rehabilitation and performance. He served as a professor of spine biomechanics at the University of Waterloo for over 30 years, where he conducted groundbreaking research into the mechanical causes of back pain and the development of evidence-based treatment strategies. Dr. McGill is renowned for his work translating complex biomechanical science into practical clinical applications, particularly for athletes and individuals with persistent low back pain. His published work, including over 240 scientific papers and best selling books, has influenced clinicians, researchers and rehabilitation professionals worldwide.
When I first became aware of Dr. McGill’s research, I was determined to eventually learn directly from him. I immersed myself in his published research, read all of his books and consumed every piece of online content I could find. After attending one of his seminars in Seattle, Washington, I immediately enrolled in a second seminar held the following weekend in Los Angeles, California. My goal was to deepen my understanding, and I suspected I might be the only attendee at both events. Before the second seminar began at the John Wooden Athletic Center, Dr. McGill stepped into the infamous memorial room. I chose to do the same in hopes of a brief face to face interaction. My ultimate goal, to learn directly from Dr. McGill one on one, was initiated as a result of my time at UCLA. Three months later, I was pulling into his driveway in Canada to spend a weekend learning directly from the "Back Mechanic" himself.
"A return to the science."

Dr. McGill, best known for developing the “McGill Big 3” core stabilization exercises, provides a progressive, individualized rehabilitation framework tailored to each of his patient’s unique needs. His approach is always preceded by an in-depth, comprehensive assessment, which guides the precise, nuanced recommendations that follow. Interestingly, despite his affiliation with the Big 3 exercises, Dr. McGill does not routinely prescribe them, an often overlooked point by those who have not studied his work in depth. Rather, his guidance is the result of a detailed 4 hour assessment, an unusually extensive evaluation that likely far exceeds most patients' prior experiences with clinical care. A critical aspect in my time working with Dr. McGill and attending his seminars is the importance of "converging on a precise diagnosis." This fundamental aspect allows all other aspects of a nuanced, comprehensive care plan to be established.
The concept of “virtual surgery” is often recommended as a strategy to temporarily eliminate movements that provoke pain, allowing the body a chance to begin healing without surgical intervention. As Dr. Stuart McGill explains, this approach, grounded in precise assessment and specific guidance, has demonstrated a success rate exceeding 95%, even among individuals who believed surgery was their only option. These outcomes, supported by patient follow-up and clinical data, emphasize the critical importance of identifying and avoiding pain triggers. Virtual surgery serves as an effective initial strategy to remove aggravating factors, followed by a carefully tailored plan of graded reduction and progressive reintroduction of movement.

Following the identification of pain provoking triggers and the initial period of "virtual surgery," the next step involves the intentional reintroduction of pain free movements. This process, referred to as graded exposure, is designed to avoid exceeding the individual's mechanical tipping point, thereby preventing further sensitization of the underlying injury. Importantly, this phase of rehabilitation mirrors the movement patterns of a healthy, pain free individual, but with a significantly reduced capacity. By framing it this way, patients can focus on rebuilding a strong, pain free foundation that supports progressive improvements over time. This approach initiates a positive cascade of benefits (physiological, anatomical and psychological) associated with safe, pain free movement and exercise by empowering the individual through a sense of control.


While Dr. Stuart McGill is widely recognized for his mechanical approach to spine health and rehabilitation, Dr. Michael Shacklock offers a complementary perspective grounded in neuroanatomy. Dr. Shacklock’s work focuses primarily on the nervous system, particularly the altered movement behaviors of nerves following injury. Through his neurodynamic approach, he emphasizes the importance of restoring normal neural mobility, often leading to meaningful reductions in pain through targeted neural mobilization techniques.
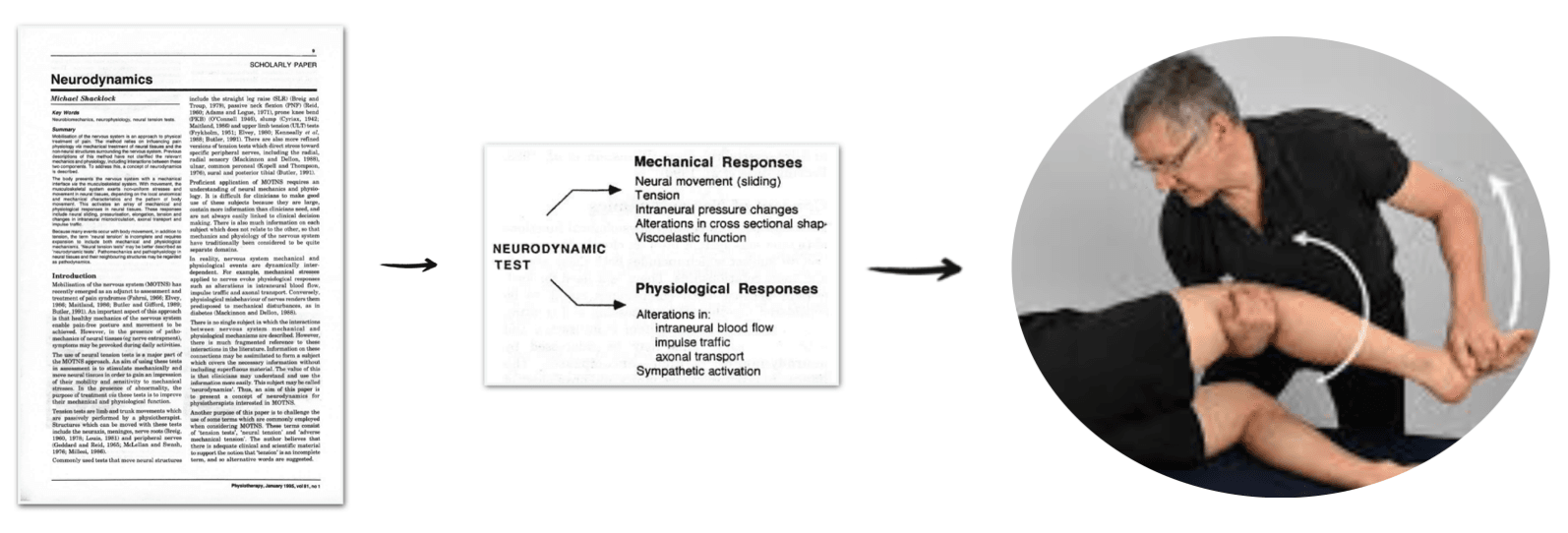
Neurodynamic techniques, including neural mobilization, have been increasingly recognized for their effectiveness in managing low back pain (LBP), particularly when associated with radiculopathy. A growing body of peer reviewed literature supports their role in reducing pain, improving function and enhancing quality of life for patients with LBP. Several related approaches in pain management and rehabilitation are based on neurodynamic principles. Commonly prescribed techniques such as neural flossing and ELDOA serve both diagnostic and therapeutic purposes, aiming to restore optimal nerve mobility and function. Dr. Shacklock’s neurodynamic approach focuses on reestablishing preexisting and in some cases, introducing novel movement patterns in previously impaired nerves. Due to the high degree of nuance involved in proper assessment and application, Dr. Shacklock’s techniques are best implemented by a clinician with formal training in neurodynamics or after a substantial educational period.
It's important to recognize that neurodynamic techniques often serve as a supplemental component within the broader rehabilitation process. When integrated with a structured approach (thorough assessment, elimination of pain provoking triggers and graded exposure) neurodynamics can be a powerful adjunct therapy. Equally critical in rehabilitation is the timing of intervention. It is not uncommon for a movement or modality that initially exacerbates symptoms to become therapeutic when reintroduced later in the recovery timeline. In the case of neural mobilization techniques, heightened pain sensitivity may initially prevent their use even in their most regressed forms. However, once the nervous system has desensitized, these same techniques can often be reintroduced with significantly greater effectiveness.

Dr. Sean Mackey is a prominent physician, scientist and leader in pain medicine. He serves as Chief of the Division of Pain Medicine and director the Stanford Pain Management Center, one of the nation’s largest and most advanced centers for comprehensive pain care. Dr. Mackey’s research centers on uncovering the biological and neurological mechanisms underlying chronic pain and developing innovative, evidence based treatments. He also leads the Systems Neuroscience and Pain Laboratory (SNAPL), where his team uses cutting edge neuroimaging, psychophysics and behavioral science to better understand and manage chronic pain.

The brain has a built in system for detecting pain signals. One key pathway, from the thalamus to the anterior cingulate cortex, helps decide how much attention we should give to a painful sensation. The anterior cingulate also adds an emotional layer, influencing how distressing that pain feels. Another important area, the insular cortex, has two parts. The posterior region is primarily involved in interpreting interoceptive signals from the body, while the anterior portion integrates emotional and cognitive aspects of the pain experience. The amygdala and hippocampus, along with the broader stress response system, collectively influence how pain is perceived and processed, highlighting the complex interplay between physiological and psychological factors in pain modulation.
Understanding these complex pathways and their various influences on our physical, mental and emotional states, one can likely realize the opportunity to influence these pathways to either directly or indirectly modulate their effects. Often times the problem is not with all the readily available tools, rather it is a clinician working through the right tool in the right context. These approaches, often but not always, include various attempts to incorporate pain management medications. Shockingly, there are over 200 medications that have been shown to have analgesic properties.

As Dr. Mackey has candidly mentioned, many pharmaceutical agents used in pain management are borrowed from other medical specialties. For instance, certain antidepressants have demonstrated efficacy in modulating pain related circuits in the brain, beyond their traditional role in mood regulation. Similarly, anti-seizure medications (commonly used in neurology) affect ion channels and other neuromodulatory systems involved in pain signaling. Additionally, some anti-arrhythmic drugs prescribed by cardiologists are potent sodium channel blockers, targeting the same channels responsible for generating nerve impulses. Recognizing the cross disciplinary therapeutic potential of these medications allows clinicians to expand their treatment toolkit and develop a more nuanced, individualized pain management strategy. Notably, an interesting class of medications, Tricyclic antidepressants (TCAs) are primarily used to treat depression, but also effective in managing certain types of chronic pain, especially neuropathic pain. Because TCAs hit multiple receptors in the brain, they have proven to be more effective in pain management.

A recurring focus in discussions about pain perception and modulation is the role of descending pathways, particularly those originating from the rostral ventromedial medulla (RVM). While a detailed exploration of these pathways is beyond the scope of this article, it’s important to recognize that effective treatment of psychological symptoms does not, on its own, confirm that pain is purely psychological in origin. Despite the existence of over 200 known analgesic compounds, only a small number are FDA approved specifically for pain management. Many commonly used medications such as the previously mentioned TCAs, anticonvulsants and other drugs developed for psychiatric or neurological conditions are prescribed off label for pain. It should once again be mentioned, the level of a person's self efficacy, underlying mood disorders and catastrophizing tendencies are all additional factors that play a role in one's ability to manage pain.


A recurring theme that emerges across workshops, seminars, conventions and one on one learning experiences is the gap between what patients receive and what they truly want. The desire to be heard consistently emerges are the highest priority. Patients consistently express the need for their healthcare provider to fully understand their perceptions and experiences. Dr. Stuart McGill, for example, conducts a comprehensive four hour assessment with each patient, something I personally experienced. During our session, we discussed my medical history, reviewed my MRI together and collaboratively explored both the clinical findings and my own narrative. This approach exemplifies the kind of patient centered care that fosters trust and meaningful outcomes.

*The photos above are taken from my 1-on-1 time with Dr. McGill at his home in Canada (2018).
An underwhelming aspect of a traditional medical visit is the brevity of time spent with the clinician or doctor. As an absolute imperative point in one's comprehensive plan, a thorough assessment is the foundation on which all other nuance aspects build. Often times, one's pain is dynamically trigger and revealed during an assessment; however, may go unnoticed in a brief discussion or static imaging (traditional MRI). These dynamic pain triggers are often revealed and confirmed in two ways. The first, through provocative testing, where a patient intentionally elicits their pain to reveal a causal mechanism. The second, through video fluoroscopy (real time video X ray), where the structural pathology is revealed in the anatomical position a patient reports pain. This presentation is particularly common in cases of spinal instability and often offers psychological relief to patients whose MRIs have failed to reveal a clear diagnosis. It serves as a critical reminder that imaging should be viewed as one component of a comprehensive assessment. This also emphasizes the importance of working with a qualified clinician to avoid one's pain as being mischaracterized as “idiopathic,” “nonspecific” or reduced to purely psychological.
Following a comprehensive, individualized assessment, patients are provided with a clear baseline of their current functional status. Once specific goals are established, whether related to quality of life, return to daily activities or competitive performance, the gap between present capacity and desired outcomes becomes apparent. Bridging this gap involves the strategic use of graded exposure, carefully designed to avoid surpassing the individual's mechanical tipping point. Progressively overloaded training strategies can then be introduced, tailored to the patient’s tolerance and recovery capacity. This phase demands precision, and it is often where a highly skilled trainer or clinician delivers the greatest value by guiding safe, incremental progress without exacerbating the condition.
Introducing a structured educational phase during rehabilitation is also crucial for long term recovery and injury prevention. One of the leading contributors to repeat injuries is a lack of patient understanding regarding the nature of their injury, the specifics of the intervention and the resulting implications. For example, a healthy intervertebral disc is typically not innervated and can distribute mechanical loads evenly both at its own level and across adjacent segments. However, this changes once the disc becomes structurally compromised. An injured disc may develop nerve innervation and altered load distribution, leading to compensatory motion in adjacent segments. Without targeted movement retraining, patients often compensate for the loss of mobility at the injured site by increasing motion in the segments above or below. When this compensation occurs alongside poor motor control, it can place excessive stress on these adjacent areas, increasing the likelihood of reinjury. Educating patients about these biomechanical changes and guiding them through proper movement strategies is essential to breaking this cycle and promoting sustained recovery.

Importantly, chronic pain management typically requires a multidisciplinary approach across six key areas. Medications (NSAIDs, antidepressants and anticonvulsants) help modulate pain signals when used appropriately. Nerve blocks and procedures like epidural injections offer targeted relief. Psychological therapies, including CBT and mindfulness based approaches, address the emotional aspects of pain. Physical therapy focuses on restoring movement and reducing sensitivity. Complementary approaches like massage therapy, acupuncture and nutraceuticals may offer additional support. Finally, education, self empowerment and skill building are critical for long term resilience and effective self management.
Within the broader toolkit of therapeutic options, supplemental and regenerative therapies are becoming increasingly popular. Their effectiveness appears to be most valuable when used as adjuncts to a well established, evidence based treatment plan. As previously discussed, intervertebral discs are composed of interwoven collagen fibers, supporting the rationale for including collagen supplements, or endogenous collagen enhancing agents, as part of a comprehensive care strategy. Although the market for collagen supplements has expanded significantly, a key consideration is their pairing with vitamin C, which has been shown to independently and synergistically support collagen synthesis.
Additional, though less thoroughly studied, interventions include therapeutic peptides, which are gaining popularity for their potential regenerative and healing effects. Among these is BPC 157, which has gained popularity for it's apparent tissue healing properties. While research on BPC 157 and other peptides is growing, much of the early evidence comes from animal studies rather than human trials, and clinical applications remain preliminary. As with any supplement or emerging therapy, the first question should always be: “Is it safe?” Once safety has been reasonably evaluated for one's specific safety and risk profile or an informed decision has been made regarding potential risks, the next consideration is, “Can you afford the wallet biopsy?” In other words, if a therapy poses no harm and is financially accessible, it may be reasonable to explore as part of a broader plan.

Low dose naltrexone (LDN), typically administered at 4.5 mg (1/10th the standard dose) has also gained attention for its potential role in pain modulation. While traditionally known as an opioid receptor antagonist, LDN also inhibits Toll-like receptor 4 (TLR4) on microglia, the non-neuronal immune cells of the CNS. Microglia become activated in response to stress or injury, releasing pro-inflammatory mediators that contribute to pain sensitization. By blocking TLR4 signaling, LDN is thought to dampen this neuroinflammatory cascade, potentially reducing pain perception and improving outcomes in certain chronic pain conditions.
Prolotherapy is an injection treatment intended to stimulate the body’s natural healing processes. It typically involves administering a solution of dextrose, saline and anesthetic directly into damaged or weakened connective tissue. This targeted irritation induces a mild, localized inflammatory response, which activates the immune system and initiates a cascade of tissue repairing processes. While inflammatory mediators such as prostaglandins, histamines and interleukins are often viewed negatively, they play essential roles in this process when present in controlled amounts. Their release signals the recruitment of repair cells, platelets, growth factors and specialized proteins to the site of injury. This response promotes the deposition of new collagen, gradually restoring the structural integrity and function of the affected tissue. Multiple treatment sessions are typically required to achieve optimal outcomes. Importantly, anti-inflammatory medications may suppress this beneficial inflammatory response and are often avoided during this period.

I received 2 comprehensive treatments (2017 & 2019) of prolotherapy, platelet rich plasma and platelet lysate.
Platelet-Rich Plasma (PRP) is a regenerative biologic treatment derived from a patient's own blood. Platelets, often referred to as the body’s natural repair cells, contain an abundance of bioactive proteins and growth factors that are essential for initiating and accelerating tissue repair and regeneration. These growth factors play a key role in connective tissue healing, new blood vessels formation (angiogenesis) and the overall wound healing process. PRP is commonly used as a non-surgical intervention to promote healing in soft tissue injuries. More recently, PRP serves a vital role as an adjunctive therapy in post-operative care to enhance recovery. To harness the therapeutic potential of platelets, they are concentrated through centrifugation, significantly increasing the levels of growth factors. When injected into injured ligaments, tendons or joints, PRP can stimulate a localized and natural healing response, effectively enhancing the body’s intrinsic repair mechanisms.

An understanding of the foundational scientific principles is essential in injury recovery. No psychological workaround, cutting edge orthobiologic or experimental therapy can override the anatomical, mechanical and biological realities of how injuries occur, heal and recover. Adjunct treatments, while powerful if used appropriately, are most effective when used to support a well designed, evidence based protocol. For example, investing in platelet rich plasma (PRP) therapy may offer benefits, but if the recovery process involves activities that continue to irritate or sensitize the underlying issue, meaningful progress is unlikely. This is often not due to defiance or noncompliance, but simply a lack of awareness and understanding that ultimately impedes recovery. Education, preferably in a easily understood format, leads to patient empowerment and self efficacy. Drawing on my personal experience, the most effective elements of my recovery toolkit included carefully structured graded exposure, high quality bodywork through skilled massage therapy, behavior change supported by strategic exercise modifications, and allowing time and natural healing processes to work, especially when supported by regenerative biologic interventions. It is also important to note the often underutilized psychological supporting therapies, notably CBT and MBSR.
One cannot neglect the psychological contributors to, and compounding of, physical pain. Psychological tools, most notably cognitive behavioral therapy, has promising adjunct treatment potential. A wise approach is to consider the pillars of health, regardless of pain status, as a continual set of dimmer switches. Rarely all the way turned up, never turned off. This orchestrated approach allows continual progress in conjunction with the body's ability to heal. Prioritizing psychological coping strategies, strategically introducing professionally guided movement practices and thoughtfully balancing stress to adaptation ratios provides the strongest foundation for success. As Dr. Mackey emphasizes, the nuance lies not in the specific modality chosen, but in how different approaches are combined and tailored to the individual.

- Stretching will decrease my back pain.
- Although stretching is often an advisable training tool, in the instance of someone with acute back pain stretching is often detrimental. When stretching, the muscle spindle sends an afferent nerve signal to the brain, causing temporary relaxation and potential pain alleviation. Unfortunately, you are also simultaneously contributing to the root cause of your pain, which is likely disc in origin. This is liken to scratching an itch or picking a scab. The temporary benefit perpetuates the underlying issue. Of course, when the itch subsides or the scab heals, you are able to do as you please.
- An alternate solution is neural flossing. "Flossing" the nerve roots with gentle flexion and extension techniques allow the nerves to glide along their natural pathways without compromising anatomical position. Neural flossing is both diagnostic and therapeutic. For those who find success in this technique, it is a large contributor to their relief. Massage therapy also is an amazing option during these particular scenarios. Targeted muscle release without compromising one's anatomical position is often an overwhelming positive addition to one's care plan.
- Non-specific, generalized pain is a common contributor to back discomfort/disfunction.
- Most, and potentially all, pain has a specific origin(s). Only when appropriately diagnosed, often through a comprehensive hands on assessment, does one successfully differientiate signal from noise. A commonly frustrating scenario many face is having never originally identified their pain contributors. This often elevates the volume of one's pain, making additional or most movements painful. This is likely a major contributor to the commonly self diagnosed "non specific" or "general" pain. A failure to identify the primary contributor(s) to one's pain results in additional contributors to pain.
- If your pain fluctuates in severity, it like has a cause. A helpful solution is to first calm things down, which is often the purpose behind Dr. McGill's "virtual surgery." The next strategy is differentiate signal from noise and accurately identify one's pain contributors. The following, and indefinite, strategy is to implement graded exposure designed to gradually restore your robust functionality. Calm things down. Build things up.
- Pain experiences are relatively similar for every individual.
- A common misconception is the inaccurate assumption that static imaging (such as traditional MRI scans) directly reflects how a person should or does feel. While MRI findings can provide valuable insights, they represent just one piece of the diagnostic puzzle. Their greatest utility often lies in contributing to a comprehensive clinical assessment, rather than serving as a standalone indicator of pain or function.
- Pain is a highly subjective experience, influenced by far more than just observable physical pathology. In addition to structural or tissue related issues, which can be difficult to quantify, there are numerous invisible factors that shape an individual's perception of pain. These include psychological, emotional and social influences, all of which contribute to the complexity of assessing and treating pain effectively.

Few factors impair long term health and quality of life more significantly than chronic pain. Getting injured is asymmetrically harmful, and much more so as we age. Injury is often the catalyst to physical, psychological and metabolic deconditioning. Pain management is a meaningful mission with disproportionately positive outcomes. In that sense, it represents a problem truly worth solving. Fortunately, the work of the professionals referenced above have provided a strong foundation upon which to build future strategies.
A critical challenge for the future lies in developing a world class, integrated healthcare network. This would include a data driven, intelligent online platform capable of processing clinical nuance, contextual factors, standards of care and patient outcomes. Artificial intelligence (AI) will likely play a key role in this evolution, enhancing both patient and provider access to personalized, evidence based care that was previously difficult or impossible to achieve. Emerging technologies such as digital twins, real time health record integration and AI assisted drug development can further enhance clinical decision making, while enabling patients to collaborate with the provider of their choice through accurate, dynamic and transparent data.







